
Eosinophilic myenteric ganglionitis presenting with constipation and erythema ab igne: a case report
Highlight box
Key findings
• Chronic abdominal pain may present with erythema ab igne.
• Following total proctocolectomy the symptoms and erythema ab igne resolved, and histopathology confirmed eosinophilic myenteric ganglionitis (EMG).
What is known and what is new?
• EMG is a rare and still poorly understood entity. It has been hypothesized as one cause of chronic intestinal pseudo-obstruction.
• This manuscript adds one more case of this rare disease with an uncommon presentation.
What is the implication, and what should change now?
• Severe ongoing constipation and abdominal pain may represent the manifestation of a yet unknown enteral neurological neuropathy. In such cases we recommend colorectal surgery referral.
Introduction
Eosinophilic myenteric ganglionitis (EMG) is an uncommon but significant disorder of the intestinal neuro-musculature (1). The condition constitutes a histological subtype of the enteric neuropathies (disorders of enteric neurons) which have been associated with a number of gastrointestinal motility disorders such as chronic intestinal pseudo-obstruction (CIPO), chronic constipation, achalasia and gastroparesis (2,3). Enteric neuropathies are themselves part of a greater spectrum of gastrointestinal motility disorders that also include enteric myopathies and mesenchymopathies, disorders of the intestinal smooth muscle and interstitial cells of Cajal respectively (3).
EMG has been described primarily in relation to cases of CIPO, which presents clinically as an apparent mechanical bowel obstruction in the absence of an actual occlusive lesion of the bowel lumen (4). Neuropathic causes of CIPO may be further classified as being inflammatory, characterised by the inflammatory cell infiltration of the ganglionated enteric nervous system plexi with particular involvement of the myenteric plexus, or non-inflammatory, typified by neuronal degeneration and loss (5). EMG falls into the category of inflammatory enteric neuropathy, although the inflammatory cell infiltrate in myenteric ganglionitis is much more commonly CD3+ lymphocyte-predominant (6). Eosinophilic and mast cell-predominant inflammatory neuropathies are far rarer and hence less well-characterized, although eosinophilic ganglionitis has been noted to be associated less with neuronal degeneration than lymphocytic ganglionitis (6). We report a case of EMG in an adult woman. We present this case in accordance with the CARE reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-24-17/rc).
Case presentation
A 63-year-old woman presented with abdominal pain and a 3-year history of severe constipation that had been worsening over the preceding year with poor response to laxatives. At presentation, the patient had a striking pattern of reticular pigmentation across her abdomen consistent with a diagnosis of erythema ab igne (Figure 1). This was attributable to her long-term nightly use of a hot water bottle on her abdomen in an attempt to relieve her severe generalised abdominal pain. A gastroscopy and colonoscopy had failed to identify a clear cause for the obstructive symptoms, and the patient’s medical history was notable primarily for gastro-oesophageal reflux disease, Barrett’s esophagus, hypertension and previous shoulder surgery.

Investigations, including a colonic transit study, defecating proctogram, anorectal physiology, anorectal manometry, and imaging in the form of both ultrasound and computed tomography (CT), were unsuccessful in identifying a clear cause for the patient’s symptoms. A moderate anterior and small posterior rectocele were identified on the defecating proctogram. A trial of biofeedback in the form of aperients failed to provide symptomatic improvement and resulted in increased abdominal pain.
Due to the ongoing severity of her generalised abdominal pain associated with her constipation, the patient expressed a desire for an initial colostomy formation, having a grand-daughter who had undergone a similar procedure for a gastrointestinal disorder a year earlier. The child had also presented with intractable abdominal pain associated with severe constipation.
Due to persistent symptoms, the patient was eventually managed with a total of three surgical procedures, each approximately a year apart. The first of these was an end-loop colostomy that brought an initial period of relief from chronic generalised abdominal pain, before intermittent proximal obstruction of the stoma and mucous obstruction of the rectosigmoid stump requiring manual disimpaction became troublesome. An abdominoperineal resection of the rectosigmoid stump with a revision colostomy and appendectomy was therefore performed to address these issues, but the patient was still troubled by significant obstructive dysfunction of the stoma and abdominal pain. A total colectomy with end ileostomy was eventually performed, and, at post-operative follow-up, the patient was found to have had improvement in symptoms and good satisfaction with the end ileostomy which was functioning well. Her abdomen was soft and non-tender to examine, with resolution of the erythema ab igne twelve months after the operation.
Pathologic findings
Histopathological evaluation of surgical specimens from the end-loop colostomy and abdominoperineal resection was largely unremarkable with respect to explaining the patient’s obstructive symptoms and pain. The abdominoperineal resection included a 325-mm length of sigmoid colon, rectum and anus with mesocolon and mesorectum, and revealed diverticula in the sigmoid colon with associated thickening of the muscularis propria and narrowing of the bowel lumen. No significant inflammation or evidence of malignancy was identified. The appendiceal specimen resected at the surgery showed neutrophils within the submucosa and muscularis propria and focal mucosal erosion of the appendix consistent with acute appendicitis.
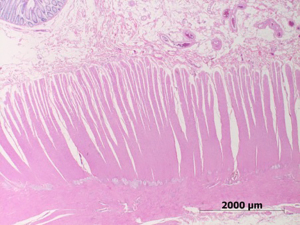
The subsequent total colectomy and end ileostomy comprised a 500-mm length of colon from the caecum to descending colon with 30 mm of terminal ileum. Macroscopically, the mucosal surface was largely unremarkable except for the presence of three tubular adenomas with low-grade dysplasia. There was no evidence of diverticulitis and the serosal surface appeared unremarkable. Microscopically, diffuse melanosis coli of the bowel was noted, without inflammation or ulceration of the mucosa. The myocytes of the longitudinal and circular layers of the muscularis propria were unremarkable with no inclusions or areas of fibrosis present. There was, however, focal prominence of the myenteric plexus, with eosinophils present in the myenteric plexus plus a small number of eosinophils in the surrounding muscularis propria (Figure 2). Eosinophils were not increased in the mucosa or submucosa, and no apparent hypoganglionosis was identified (Figure 3). No peripheral eosinophilia was detected in the peripheral blood. Immunohistochemical staining for S100 highlighted the prominent myenteric plexus while staining for CD117 showed scattered mast cells and a normal number of interstitial cells of Cajal. No loss of Bcl-2 expression was seen in the ganglia and there was no increase in glial fibrillary acidic protein (GFAP) staining. Immunostains for CD3 and CD20 showed few lymphocytes in the myenteric plexus or muscularis propria. These findings are consistent with EMG and provide an explanation for the patient’s obstructive intestinal symptoms.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
We have presented a case of EMG as the cause of a long-standing and severe functional obstructive bowel disorder in a 63-year-old woman. To date, we are aware of ten other cases of EMG reported in adults, five male, five female, with ages ranging from 34 to 93 years (2,7-10). The condition has also been described in the pediatric population, in six children, three male, three female, two-newborns, one 1-month-old, one 2-year-old, one 11-year-old and one 15-year-old (1,11-13). The more recent cases have evened up the gender distribution of EMG, with two cases of the condition in males who also had Hirschsprung’s disease (12,13). Of note, the grand-daughter of the patient described was also reported to have had a gastrointestinal disorder that required a colostomy at a young age, although no evidence of EMG was identifiable, which could otherwise have suggested a hereditary tendency for the condition. This women’s particular presentation with chronic abdominal pain, constipation and the defining feature of an eosinophilic infiltration of the myenteric plexus, and its reporting in other similar cases is what appears to be the cluster of symptoms, signs and pathological abnormality that defines EMG.
In contrast to previous existing adult presentations of EMG, which featured specific acute or subacute episode of obstructive symptoms with radiologic evidence of colonic dilatation at presentation (2,7), the patient we describe presented with a more progressive, though still severe, course of constipation and abdominal pain in absence of radiologically identifiable bowel pathology.
The patient’s presentation was also notable for being associated with the unusual physical finding of erythema ab igne of the abdomen. Erythema ab igne is a cutaneous clinical sign featuring an area of erythematous reticular hyperpigmentation secondary to repeated exposure of the skin to infra-red heat radiation below the burn threshold (14,15). The pigmentation is thought to arise from damage to dermal vasculature with associated vasodilation and deposition of hemosiderin (15). Erythema ab igne has historically been associated with excess proximity to fires, but has since been described in relation to a range of processes from exposure to heaters and laptops to long-term heat application for pain associated with pancreatitis or malignancies (14). The sign has also been reported as a potential indicator of serious disease, having been described in association with pancreatic and rectal cancers as a presenting feature, often secondary to the use of a hot water bottle for pain relief, prior to diagnosis (16,17), and also similarly as part of the initial presentation of inflammatory bowel disease (18). We have presented here the first known incidence of erythema ab igne occurring as a presenting feature of EMG, illustrating the importance of recognising the sign as a possible indicator of serious underlying pathology, particularly of the abdomen. We acknowledge though that erythema ab igne is in clinical practice a sign usually associated with chronic abdominal pain and hot water bottle use, but not pathognomonic of any particular pathological entity.
Histologically, the case of EMG that we have presented is, as for previous cases, characterised by the defining feature of an eosinophilic infiltration of the myenteric plexus. The bowel specimen described was remarkable mainly for the presence of a small number of eosinophils within the myenteric plexus and adjacent muscularis propria, without an increase of eosinophils in the mucosa or submucosa. As for one other adult case of EMG and most of the pediatric cases, no overt hypoganglionosis was detected in the specimen we describe. An immunostain for S100, however, did reveal a prominent myenteric plexus. It is worth noting, however, that the other of the two adult cases of EMG that we are aware of described a considerably different disease phenotype in which CD4+ lymphocytic infiltration with hypoganglionosis of the myenteric plexus occurred in addition to the eosinophilic infiltration, with eosinophilic involvement of the mucosa as well (7). Interestingly, no peripheral eosinophilia was noted for the patient we describe.
Consistent with the histological picture of an enteric neuropathy, a stain for smooth muscle actin in the bowel specimen we have presented was normal, and a stain for CD117 showed a normal number of interstitial cells of Cajal. As for other cases of EMG, the mucosa was free of ulceration or inflammation. Diffuse melanosis coli was noted, however, most likely secondary to the patient’s long-term use of laxatives, and, along with the erythema ab igne secondary to heat-mediated pain relief, offers a physical indication of the chronicity and intractability of the patient’s symptoms.
Disappointingly, the pathophysiology of EMG remains unclear, although the expression of interleukin-5 demonstrated within enteric neurons of a set of pediatric patients with the condition has suggested a possible role for the mediator in disease pathogenesis (1). As neuronal damage does not typically feature in the condition, proposed mechanisms for the associated gut dysmotility have included direct functional limitation caused by the eosinophilic infiltrate or dysfunction mediated by potential humoral effectors from the eosinophils (6). The reason for the apparent preferential targeting of the myenteric plexus also remains unclear (5).
EMG has been hypothesized as one cause of CIPO, further classified into inflammatory and degenerative neuropathies, diseases of the interstitial cells of Cajal, or smooth muscle cells (7). EMGs putative mechanism is suggested to commence as a systemic immune reaction progressing into a chronic inflammatory lesion (7).
Nonetheless, the case of EMG that we have presented, in addition to the previous existing cases, illustrates the need for improved characterization of the condition and the importance of considering it, as well as other related neuropathies, as differentials in cases of functional gut dysmotility. The non-emergent and non-specific nature of the case we present here, in contrast to the two adult presentations to the emergency department previously described, raises the possibility that the condition may potentially be an undiagnosed cause of cases of functional bowel disorder. Treatment of the condition has included the use of systemic steroids and immunosuppressants or anti-inflammatory drugs such as azathioprine, sulphasalazine or 5-aminosalicylate, which have been reported in pediatric cases to successfully aid resolution of symptoms (1,11). The adult cases of EMG so far have only involved surgical intervention in management, but it is feasible that with improved detection of the condition, this may perhaps become more avoidable in the future (11,12).
Conclusions
We have presented a rare case of EMG in an adult woman featuring a history of chronic constipation and abdominal pain in association with the striking clinical feature of erythema ab igne of the abdomen. The condition is histologically characterized by the presence of an eosinophilic infiltrate within the myenteric plexus of the intestine, although disease pathophysiology remains ill-defined and incompletely-understood. Further characterization of EMG and similar enteric neuropathies like this will be valuable in aiding detection and management of the condition in the future.
Acknowledgments
We thank Dr. Caroline Cooper for her involvement with the original histopathological report of this case.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-24-17/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-24-17/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-24-17/coif). C.J.Y. serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from December 2023 to November 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schäppi MG, Smith VV, Milla PJ, et al. Eosinophilic myenteric ganglionitis is associated with functional intestinal obstruction. Gut 2003;52:752-5. [Crossref] [PubMed]
- Chander B, Fiedler P, Jain D. Eosinophilic myenteric ganglionitis: a case of intestinal pseudo-obstruction in a 93-year-old female. J Clin Gastroenterol 2011;45:314-6. [Crossref] [PubMed]
- Knowles CH, Lindberg G, Panza E, et al. New perspectives in the diagnosis and management of enteric neuropathies. Nat Rev Gastroenterol Hepatol 2013;10:206-18. [Crossref] [PubMed]
- De Giorgio R, Sarnelli G, Corinaldesi R, et al. Advances in our understanding of the pathology of chronic intestinal pseudo-obstruction. Gut 2004;53:1549-52. [Crossref] [PubMed]
- De Giorgio R, Cogliandro RF, Barbara G, et al. Chronic intestinal pseudo-obstruction: clinical features, diagnosis, and therapy. Gastroenterol Clin North Am 2011;40:787-807. [Crossref] [PubMed]
- Antonucci A, Fronzoni L, Cogliandro L, et al. Chronic intestinal pseudo-obstruction. World J Gastroenterol 2008;14:2953-61. [Crossref] [PubMed]
- Lee H, Kang D, Kim H, et al. Unusual Histology of Eosinophilic Myenteric Ganglionitis: A Case Report. J Pathol Transl Med 2017;51:320-4. [Crossref] [PubMed]
- Kim A, Roberson JL, Maguire LH, et al. Eosinophilic Myenteric Ganglionitis Presenting as Sigmoid Volvulus: A Brief Report. Am Surg 2023;89:5021-3. [Crossref] [PubMed]
- Mitra S, Ayyanar P, Purkait S, et al. Clinical and Histopathological Spectrum of Adult Gastrointestinal Inflammatory Neuropathy. Int J Surg Pathol 2021;29:246-56. [Crossref] [PubMed]
- Akazawa Y, Hayashi T, Saito T, et al. Histological characteristics of eosinophilic myenteric ganglionitis: an under-recognised cause of chronic intestinal pseudo-obstruction. Virchows Arch 2019;474:395-400. [Crossref] [PubMed]
- Ooms AH, Verheij J, Hulst JM, et al. Eosinophilic myenteric ganglionitis as a cause of chronic intestinal pseudo-obstruction. Virchows Arch 2012;460:123-7. [Crossref] [PubMed]
- Phillips MR, Samuel J, Woosley J, et al. Eosinophilic myenteric ganglionitis with concomitant Hirschsprung’s disease: Case presentation and review of the literature. J Pediatr Surg Case Rep 2013;1:429-31. [Crossref]
- D’Auria E, Calcaterra V, Maestri L, et al. Case Report: Eosinophilic Myenteric Ganglionitis in a Child With Hirschsprung’s Disease: A Challenge in Pseudo-Obstruction. Front Pediatr 2020;8:617309. [Crossref] [PubMed]
- Tan S, Bertucci V. Erythema ab igne: an old condition new again. CMAJ 2000;162:77-8. [PubMed]
- Cabrera Hernández A, Beà Ardebol S, Medina Montalvo S, et al. Erythema ab igne. Reumatol Clin 2016;12:233-4. [Crossref] [PubMed]
- Bunick CG, King BA, Ibrahim O. When erythema ab igne warrants an evaluation for internal malignancy. Int J Dermatol 2014;53:e353-5. [Crossref] [PubMed]
- Molina AR, Behar N, Bhardwaj R. Rectal cancer presenting with erythema ab igne. JRSM Short Rep 2010;1:48. [Crossref] [PubMed]
- Tighe MP, Morenas RA, Afzal NA, et al. Erythema ab igne and Crohn’s disease. Arch Dis Child 2008;93:389. [Crossref] [PubMed]
Cite this article as: Lin AA, Kench J, Young CJ. Eosinophilic myenteric ganglionitis presenting with constipation and erythema ab igne: a case report. Ann Laparosc Endosc Surg 2025;10:8.


