Strategy of laparoscopic suprapancreatic lymph node dissection for advanced gastric cancer
Introduction
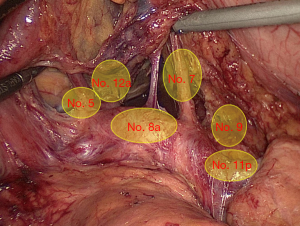
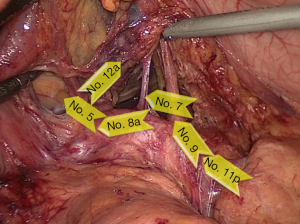
The lymph nodes (LNs) that distribute along the celiac artery (CA) system in the suprapancreatic area include LNs around the root of the left gastric vessels (No. 7, No. 8a, No. 9 and No. 11p) and the right gastric vessels (No. 5 and No. 12a) (1) (Figure 1). There is a high rate of lymph node metastasis (LNM) in this area (No. 5, 7, 8a, 9, 11p, and 12a) for patients with advanced gastric cancer (AGC). We retrospectively analyzed the clinic and pathological features of 1,551 cases with AGC, and the result showed the suprapancreatic LNM rate was 51.8% (804/1,551) (2) (Figure 2). Based on the 3th edition of Japanese Gastric Cancer Treatment Guidelines, complete clearance of LNs in the suprapancreatic area is crucial importance during radical gastrectomy with D2 LN dissection for gastric cancer (3). Clinically, LN dissection in this area is both greatly important and technically demanding for laparoscopic radical gastrectomy for patients with gastric cancer.
Operative approach to suprapancreatic lymphadenectomy
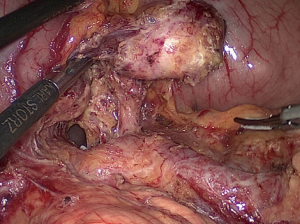
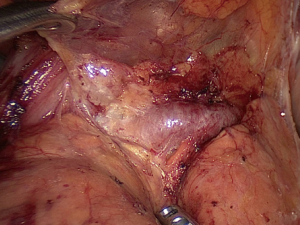
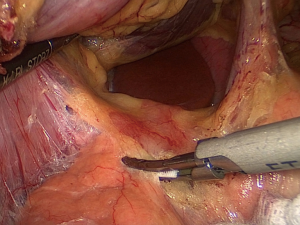
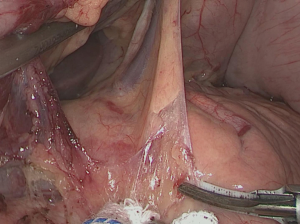
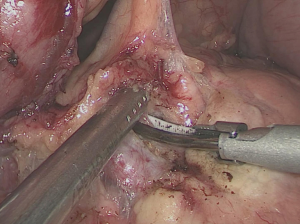
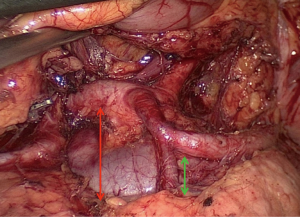
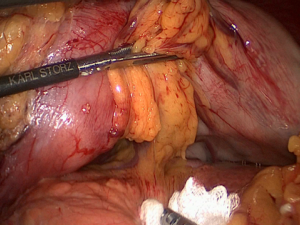
Selecting the appropriate surgical approach is the beginning of successful surgery, and also the premise of smooth procedure in laparoscopic radical resection for gastric cancer. We dissected the suprapancreatic LNs using a left approach during laparoscopic gastrectomy with D2 LN dissection for gastric cancer (4). In this approach, the initial segment of the splenic artery (SpA) was firstly exposed at the posterior pancreatic space on the left side of gastropancreatic fold (GPF) (Figure 3). From left to right, we removed the No. 11p LNs at first, then followed by the No. 9, 7 and 8a LNs. And the removal of the No. 5 and 12a LNs was completed finally (Figure 4). Lymphadenectomy in each station in this order would provide convenience for subsequent station. During this procedure, we don’t transect the duodenum from the beginning in order to ward off the left lateral liver by using the hepatogastric ligament, by this way we denude the vessels and remove fatty lymphatic tissue from the rear of the stomach (Figure 5).
Patient’s position and surgeons’ locations
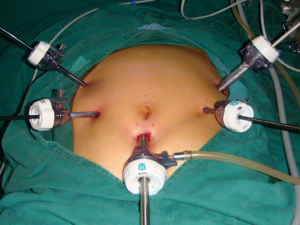
The patient is commonly maintained in the supine position with two legs separated. The operating table inclines about 10°–20° into the reverse Trendelenburg position (Figure 6). Generally, the surgeon and the assistant stand on the patient’s left and right side, respectively. While the camera operator located between the patient’s legs (Figure 7). Five trocars are usually inserted in patient’s abdominal wall (Figure 8).
Advantages of the left approach
In our center, the initial segment of the SpA is chosen as the ideal approach for the LNs dissection in the suprapancreatic area mainly based on the following five reasons (2,4,5); firstly, its location is relatively constant with less anatomic variation and as well larger diameter (Figure 9); secondly, it is located the closest to the suprapancreatic border and thus easy to be exposed after the pancreatic capsule being peeled off (Figure 10); thirdly, there is a low risk of bleeding because of fewer branching vessels in this area, and which provides a large operating field and clearly exposed vision after the dissection of No. 11 LN (Figure 11); fourthly, the initial segment of the SpA may serve as the anatomic landmark for further rightward exposing the CA, the left gastric artery (LGA) and the common hepatic artery (CHA) (Figure 12); lastly in our previous literature, the result showed there was the lowest rate of LNM in No. 11p LN among all the suprapancreatic LNs, which would decrease the difficulty of lymphadenectomy here (2).
Procedure of suprapancreatic area LN dissection
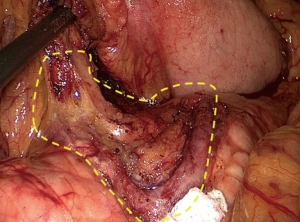
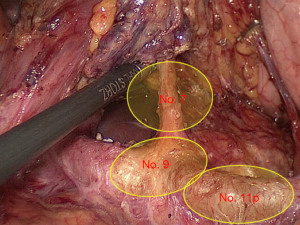
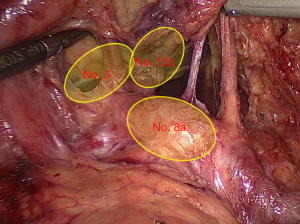
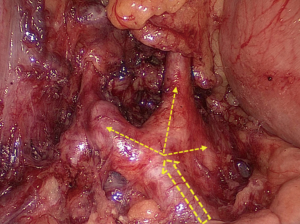
The application of reasonable and programmed procedure would simplify the operation process, which makes the complex laparoscopic surgery simple and routine, and further improves the operation efficiency. In order to enable the procedure to achieve routinization, we separate the process of LN dissection in the suprapancreatic area with a left approach into two steps (4,6). The first step is to remove the left-side LNs in this area including No. 7, No. 9 and No. 11p (Figure 13), and the second step is to remove the right-side LNs in this area including No. 8a, No. 5 and No. 12a (Figure 14).
Dissection of the No. 7, No. 9 and No. 11p LNs
Exposure methods
Using noninvasive grasper forceps, the assistant’s left hand lifts upward the junction of upper and middle GPF, and the right hand pushes the posterior wall of duodenal bulb rightward. The operator’s left hand presses gently downward the bulging body of the pancreas with a small gauze. In this way, the GPF will be sufficiently kept tensed and the suprapancreatic area can be spread out to facilitate the LN dissection (Figure 15). During the process, the assistant’s right hand can flexibly use different techniques (such as lifting, holding, pulling, and pushing) with a forceps or an aspirator to aid the surgeon in separating and exposing the surgical field.
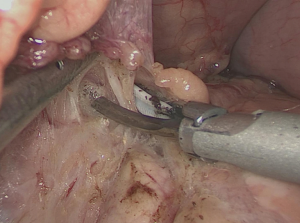
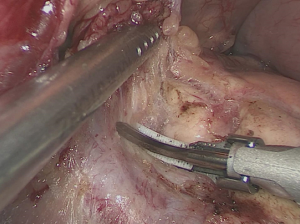
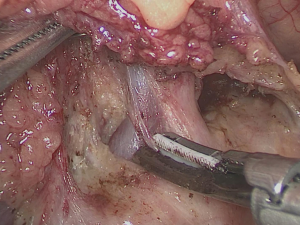
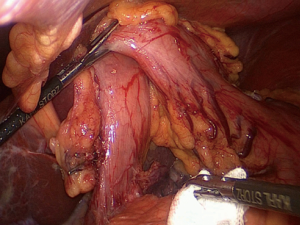
Operative procedures
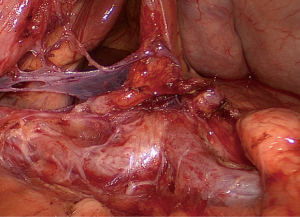
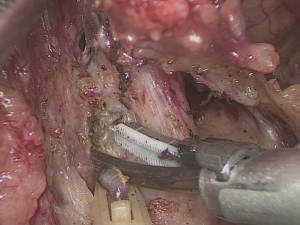
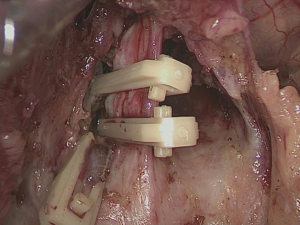
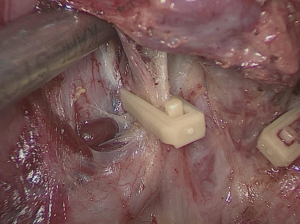
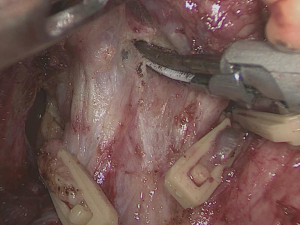
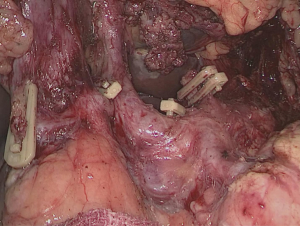
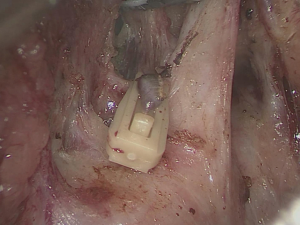
The operator uses the ultrasonic scalpel to smoothly peel off the pancreatic capsule closely on the pancreatic surface up to its superior border (Figure 16), and then open the GPF to enter the posterior pancreatic space, where the initial segment of the SpA is further separated and exposed (Figure 17). Next, the operator uses non-functional face of the ultrasonic scalpel to carefully remove the fatty lymphatic tissue along the surface of the SpA until near the posterior gastric artery (PGA), and finish the dissection of the No. 11p LNs (Figure 18). The No. 9 LNs is dissected directly from the origin of the SpA. Then, the operator uses the ultrasonic scalpel to remove fatty lymphatic tissue along anatomical space on the left edge of the CA (Figure 19) toward the crus of the diaphragm, until the left edge of the LGA root is exposed (Figure 20). Subsequently from the origin of the CHA, the operator separates and exposes the left gastric vein (LGV) along the anatomical space on the right edge of the CA (Figure 21). The connective tissues around the LGV are removed on the superior edge of the CHA, and the LGV is vascularized then divided at its root with the clips (Figure 22). After that, the operator dissects the fatty lymphatic tissue along the right edge of the CA surface (Figure 23). The LGA is then denuded on its right edge and divided at its root with the clips (Figures 24,25). With this, the dissection of the No. 7 and No. 9 LNs is completely finished.
Dissection of the No. 8a, No. 5 and No. 12a LNs
Exposure methods
Using noninvasive grasper forceps, the assistant’s left hand lifts upward the posterior wall of gastric antrum, meanwhile the right hand pushes the duodenal bulb rightward. The operator’s left hand presses gently downward the bulging head of pancreas near the fork of CHA with a small gauze. In this way, the hepatoduodenal ligament (HDL) will be kept tensed and the suprapyloric area can be sufficiently exposed at the rear of the stomach to facilitate the LN dissection (Figure 26). During the process, the assistant’s right hand can flexibly use different exposure ways to help the operator to dissect No. 8a, No. 5 and No. 12a LNs.
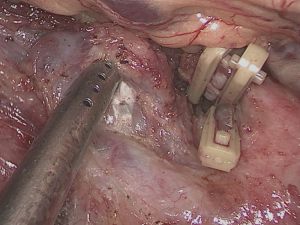
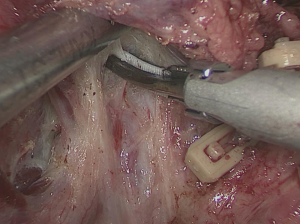
Operative procedures
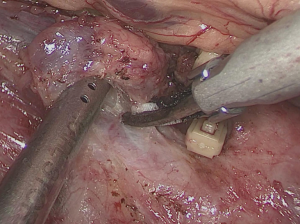
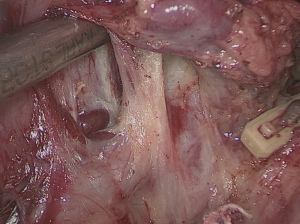
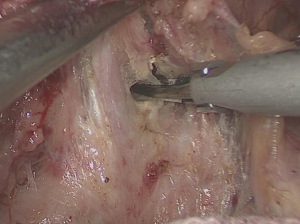
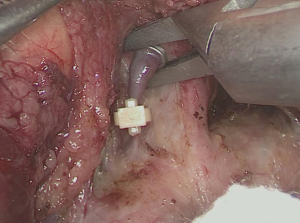
Along the anatomical space on the anterosuperior surface of the CHA, the operator uses the ultrasonic scalpel to meticulously remove fatty lymphatic tissue toward the duodenum (Figure 27), until it reaches the fork where the CHA gives off the gastroduodenal artery (GDA) and proper hepatic artery (PHA) (Figure 28). The anterosuperior LNs along the CHA is completely removed, and we finish the dissection of No. 8a LNs. From the medial border of PHA original part, the operator uses the ultrasonic scalpel to open the medial border of the HDL along the course of the PHA (Figure 29), then separate and expose the root of the right gastric artery (RGA) (Figure 30). The RGA is carefully vascularized and divided at its root with the clips (Figure 31). At this point, we finish the dissection of No. 5 LNs. Then along the anatomical space on the anterosuperior surface of PHA, the operator uses the ultrasonic scalpel to meticulously dissect fatty lymphatic tissue toward the hepatic hilum, until it reaches the fork where the PHA gives off the left and right hepatic arteries (HA) (Figure 32). The anterosuperior LNs along the PHA are removed en bloc, and we finish the dissection of No. 12a LNs. By this time, suprapancreatic LN dissection is achieved smoothly (Figure 33).
Familiar with normal anatomy and anatomic variation of suprapancreatic vessels
During the laparoscopic radical gastrectomy for gastric cancer, we should not only understand well normal anatomy and trend of perigastric vessels, but also be very familiar with their variations. Clinically, lack of sufficient understanding of vascular anatomical variations would usually cause vascular injury to bleeding and make the process of procedure unfavorable. Based on clinical practice of more than 3,000 cases undergoing laparoscopic gastrectomy in our center, we summarized the anatomical variations of perigastric vessels in detail. In our opinions, we should pay attention to two kinds of common trend and three kinds of variable trend of LGV (5-7), as well six types of replaced HA due to absence of CHA (5,8) during laparoscopic suprapancreatic LN dissection using a left approach, which facilitates surgeons to decrease the incidence of intraoperative bleeding from injured vessels and improve the surgical safety at to the greatest extent.
Summary
In summary, laparoscopic suprapancreatic LNs dissection using a left approach could be technically safe and feasible. Additionally, without transecting the duodenum might be more convenient in laparoscopic procedure for AGC. Finally, the stable team and harmonious cooperation should be the most crucial for this procedure.
Acknowledgments
Funding: The study was sponsored by the National Key Clinical Specialty Discipline Construction program of China [No. (2012)649], the Key Projects of Science and Technology Plan of Fujian Province (No. 2014Y0025) and Fund of Fujian Province science and technology innovation talents.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.09.12). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nakajima T. Gastric cancer treatment guidelines in Japan. Gastric Cancer 2002;5:1-5. [Crossref] [PubMed]
- Chen RF, Huang CM, Chen QY, et al. Why the Proximal Splenic Artery Approach is the Ideal Approach for Laparoscopic Suprapancreatic Lymph Node Dissection in Advanced Gastric Cancer? A Large-Scale Vascular-Anatomical-Based Study. Medicine (Baltimore) 2015;94:e832 [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011;14:113-23. [Crossref] [PubMed]
- Huang CM, Chen QY, Lin JX, et al. Laparoscopic Suprapancreatic Lymph Node Dissection for Advanced Gastric Cancer Using a Left-Sided Approach. Ann Surg Oncol 2015;22:2351. [Crossref] [PubMed]
- Huang CM, Zheng CH. editors. Laparoscopic Gastrectomy for Gastric Cancer: Surgical Technique and Lymphadenectomy. Netherlands: Springer, 2015:117-8.
- Huang CM, Wang JB, Wang Y, et al. Left gastric vein on the dorsal side of the splenic artery: a rare anatomic variant revealed during gastric surgery. Surg Radiol Anat 2014;36:173-80. [Crossref] [PubMed]
- Wang Y, Huang CM, Zheng CH, et al. Classification of anatomic variations in the left gastric vein during laparoscopic gastrectomy. Anat Physiol 2013;3:2.
- Huang CM, Chen RF, Chen QY, et al. Application Value of a 6-Type Classification System for Common Hepatic Artery Absence During Laparoscopic Radical Resections for Gastric Cancer: A Large-Scale Single-Center Study. Medicine (Baltimore) 2015;94:e1280 [Crossref] [PubMed]
Cite this article as: Li P, Huang CM, Zheng CH, Lin JX, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M, Tu RH. Strategy of laparoscopic suprapancreatic lymph node dissection for advanced gastric cancer. Ann Laparosc Endosc Surg 2016;1:15.