Laparoscopic anterior resection of rectal cancer with lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery (LAR-LND-PLCA)
Introduction
Colorectal carcinoma is the second most commonly carcinoma in females and the third in males. In 2012 there are about 1.4 million new cases and 693,900 deaths (1). And approximately one third of all colorectal carcinoma are rectal cancer.
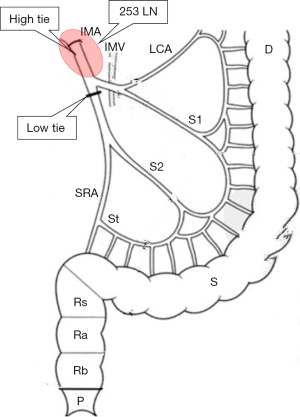
The anatomy of rectum is complex, and we need a good understanding of the anatomy of the rectum, good psychological quality, excellent surgical technique and the operation team with the tacit understanding to complete the laparoscopic anterior resection of rectal cancer with lymph node dissection around the inferior mesenteric artery (IMA) with preservation of the left colic artery (LAR-LND-PLCA). Here (Figure 1), we share the LAR-LND-PLCA surgical skills by a case of rectal cancer.
Methods
Surgical indications
LAR-LND-PLCA is suitable for the cancerous lesion located within 12 cm of the anal verge by rigid proctoscopy.
The contraindications of LAR-LND-PLCA are as follows: patients with severe cardiopulmonary in sufficiency, T4b, obstruction or tumor >6 cm in size.
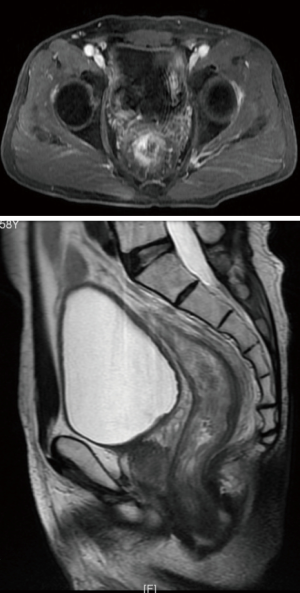
In the video, the patient is a 59-year-old man diagnosed to be moderately differentiated rectal cancer after CRT, and preoperative tumor staging was ycT3N1M0 by MR (Figure 2).
Surgical position
After anesthesia, the patient is placed in lithotomy position and Trendelenburg position. In the operation room, there are two monitors placed right above the head and between the patient’s legs. The surgeon stands on the right side of the patient. The first assistant stands on the left side of the patient. The second assistant stands on the left side of the surgeon.
Surgical procedures
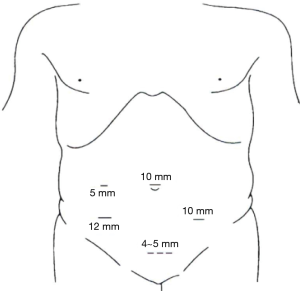
In this operation, we need five trocars, of which two 12-mm and three 5-mm trocars. Above of the navel we puncture into 12 mm trocar and put in 30 degree laparoscopy. Pneumoperitoneum was established with carbon dioxide (CO2) and the intra-abdominal pressure was maintained at a constant 12 to 15 mmHg. Other trocars were placed in position to see Figure 3. The first step is laparoscopic exploration to determine whether there was distant metastasis or spread.
And then we performed a central way to open the right side of the rectum ditch and separated the left Toldt’s fascia.
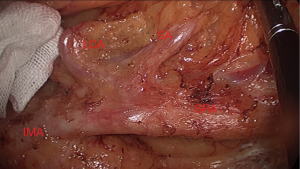
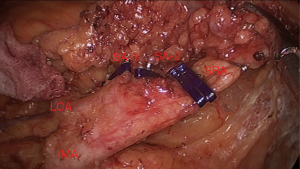
At the same time, we should dissect the lymph nodes along IMA, vein and their branch and preserved the left colic artery. After branching the left colic artery of IMA, we ligated the IMA and IMV (Figures 4,5).
Then we can free the interspaces around the rectum and cut rectum according to the TME principle.
We extended the right side abdomen 12 mm trocars hole to about 5 cm. Through this incision, we took out the rectal cancer specimens and cut the colon in the cancer proximal 10 cm, then made an end-to-end anastomosis through the anus using the anastomosis staplers.
At last, we made prophylactic ileostomy and suture the trocar holes and the incision.
Results
Operation time was 120 minutes, and the amount of bleeding was 50 mL. The postoperative pathological results showed that the poorly-differentiated adenocarcinoma with ypT2N1aM0 (IIIA) stage among which 1/14 lymph node-positive (Figures 6,7). The patient recovered well without complications and discharged from hospital 7 days after surgery.
Discussion
Some studies shows that laparoscopy is associated with the same short-term and long-term outcomes with comparing the open operations (3,4). Some scholars reported that LAR had the advantages of less bleeding, faster recovery and shorter hospital stay in the short-term endpoints (5,6). And locoregional recurrence and disease-free and overall survival are the same between laparoscopic-assisted and open operation (3,4,7,8). So LAR may be considered based on some principles in NCCN Guidelines for Rectal Cancer Version 2.2016.
Curative resection of rectal cancer included “high tie” and “low tie” of the IMA. “Low tie” included preservation of the LCA and lymph nodes dissection over the root of IMA (Figure 8). But it was controversial whether a high or low ligation of the IMA was superior. Some experts believed that there were no significant differences in the complication rate, operative time, the amount of blood loss, the number of days and OS and RFS rates between “low tie” and “high tie” with LND (9). But some scholars thought high tie may increase anastomotic leakage, because it reduced intestinal blood supply (10).
LAR-LND-PLCA LAR is a very difficult surgery and need skilled surgical techniques. So if it is difficult to deal with the problems in the laparoscopic surgery, please consult a rich experienced surgeon or change to open surgery.
Conclusions
LAR-LND-PLCA is effective and safe for the rectal cancer. Because it is too difficult, so it must be done in the rich experienced hospital.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.10.09). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional ethical approval was waived. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Zang W, Liu S, He H. LAR-LND-PLCA. Asvide 2016;3:431. Available online: http://www.asvide.com/articles/1203
- Jeong SY, Park JW, Nam BH, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 2014;15:767-74. [Crossref] [PubMed]
- Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015;372:1324-32. [Crossref] [PubMed]
- van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210-8. [Crossref] [PubMed]
- Kang SB, Park JW, Jeong SY, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 2010;11:637-45. [Crossref] [PubMed]
- Jayne DG, Guillou PJ, Thorpe H, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 2007;25:3061-8. [Crossref] [PubMed]
- Jayne DG, Thorpe HC, Copeland J, et al. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 2010;97:1638-45. [Crossref] [PubMed]
- Yasuda K, Kawai K, Ishihara S, et al. Level of arterial ligation in sigmoid colon and rectal cancer surgery. World J Surg Oncol 2016;14:99. [Crossref] [PubMed]
- Hinoi T, Okajima M, Shimomura M, et al. Effect of left colonic artery preservation on anastomotic leakage in laparoscopic anterior resection for middle and low rectal cancer. World J Surg 2013;37:2935-43. [Crossref] [PubMed]
Cite this article as: Zang W, Liu S, He H. Laparoscopic anterior resection of rectal cancer with lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery (LAR-LND-PLCA). Ann Laparosc Endosc Surg 2016;1:20.