
Pull-through and conformal resection for very low rectal cancer: a more satisfactory technique for anal function after sphincter preserving operation
When a rectal cancer is located at less than 5 cm from the anal verge (very low rectal cancer), abdominoperineal resection (APR) was generally performed (1). However, the patient’s quality of life can be compromised by the social and psychological limitations of a permanent stoma (2). Recently, intersphincteric resection (ISR) with coloanal anastomosis (CAA) and were proposed as alternative procedures to avoid APR (3-5). However, patients undergoing ISR generally have direct impairment of anal sphincter function because the anal internal sphincter, as a part of the anal sphincter complex, is removed. Moreover, dentate line is also removed resulting in an impairment of sensibility and hence also to more incontinence. Therefore, the functional outcomes of ISR or PISR remain an important issue because of sphincter damage and sensory loss (6-9).
An ideal procedure for very low rectal cancer should combine a satisfied preservation of sphincter function with oncological safety. Based on the previous study, we proposed a pull-through and conformal resection technique (PTCR) in selected patients with very low rectal cancer (9).
Inclusion criteria are: (I) well-moderately differentiated adenocarcinoma; (II) tumors located less than 1 cm from the dentate line; (III) less than 3 cm in diameter; (IV) tumors were mobile; (V) invasion of the internal sphincter but not the external sphincter and/or levator ani; (VI) no evidence of distant metastases; and (VII) patients with normal anal function before operation.
Exclusion criteria are: (I) patients underwent local excision; (II) patients with severe comorbidities.
Operative techniques
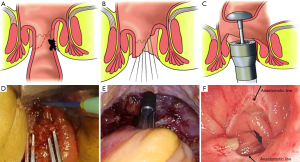
PTCR for very low rectal cancer was performed as follows. The sigmoid colon was mobilized, and inferior mesenteric artery was cut at the origin of the aorta. The rectum was mobilized until coming to the level of the dentate line between internal anal sphincter and external anal sphincter. The techniques of total mesorectal excision (TME) and autonomic nerve preservation (ANP) were used. When purse-string was finished by thick silk thread at the site of proposed anastomosis, the rectum was transected in order to pull the rectal stump through the anus. At the same time, the anal sphincter was dilated to four fingers. The sutures was held by long hemostatic forceps and inserted into the lumen of the distal rectum, and then pulled out through the anus. The rectal stump is rinsed using sterile distilled water. The proposed incisional line was made according to the tumor location and shape. The internal sphincter and dentate line of the tumor side were removed, while preserving the opposite normal rectal wall, internal sphincter and dentate line as more as possible. At the same time, the rectal stump was closed by interrupted sutures. Anastomosis was performed by a circular stapler (CDH25) at the normal rectal wall away from the denate line as far as possible (Figure 1). A protective diverting loop ileostomy was created in all patients, and was closed at 3 to 6 months after surgery if no anastomotic leakage was present.
A total of 228 patients with very low rectal cancer underwent surgical treatment (CAA group 126 patients, APR group 73 patients, and PTCR group 29 patients). There was no difference in surgical complication rate among the three groups. All patients were followed up every 3 months during the first 2 years after surgery, then every 6 months during the following 3 years, and annually thereafter. The contents of surveillance included interview of anal functions, clinical examination, chest radiography, abdominal ultrasound, and tumor markers. Colonoscopy and pelvic CT/MRI were performed every 1 year after surgery. There were no significant differences in daily fecal frequency, Wexner incontinence score, and rate of satisfactory fecal continence between the CAA and PTCR group. There were no differences in local recurrence and distant metastasis among CAA group, APR group and PTCR group.
Notes
APR with permanent colostomy is performed ranging from 25% to 35% in very low rectal cancer patients (10-12). As previous studies suggested that patients with a stoma have a poorer quality of life than those without a stoma and as many patients consider life with a permanent colostomy unacceptable (13,14). These unpleasant results of APR could be greatly improved by sphincter preservation operation. As a new sphincter preservation technique, PTCR has been used to provide promising results for avoiding permanent colostomy in patients with very low rectal cancer.
Patients undergoing the APR were more prone to develop delayed postoperative convalescence than patients receiving the sphincter preservation operation, as demonstrated by the higher rate of surgical complications and longer functional recovery (15). The higher rate of surgical morbidity in the APR patients was supposed to mainly result from the additional perineal dissection in the APR (15). In our clinical work, there were significant differences in intraoperative blood loss, operating time, and length of postoperative hospital stay between the CAA group and the APR group. There were no statistical differences in above three parameters between the CAA group and the PTCR group. The results demonstrated that PTCR for very low rectal cancer was technically feasible and safe. Also, assessment of oncological outcomes with recurrence and survival is necessary to confirm the safety of PTCR.
The central idea of PTCR is to design the excision line according to tumor location and scope and to get more normal rectal stump including the internal anal sphincter, the dentate line, and a safe incisional margin. The resection scope of PTCR includes only a part of internal anal sphincter and dentate line on the tumor side. The dentate line and sphincter complex on the opposite side is completely preserved in order to preserve the opposite rectal wall as much as possible, the anastomosis was done in the remaining wall of rectum, it’s possible to keep the anastomosis line 1 to 3 cm above the dentate line, this will much more improve the function of the anal and rectum after operation (Figure 1A-F). In this study, the distance from the anal verge of the CAA group was significantly higher than that of the APR group and PTCR group. However, there was no significant difference between the APR group and PTCR group. It is well known that postoperative anal function is strongly associated with rectal stump length. There was no different in postoperative anal function between the PTCR group and CAA group. Our results suggested that PTCR got equal preservation of anal function as CAA group in very low rectal cancer patients by appropriate preoperative selection.
As previous mentioned, the key point of successful PTCR is appropriately selection of patients. This kind of procedure has strictly indications. Firstly, it is adopted only when the very low rectal cancer showed absence of external sphincter and levator ani involvement. Secondly, it should be restricted to tumors less than 3.0 cm in diameter. The rectal stump bearing the tumor must be pulled out of the narrow anal canal during the procedure, the excision should be under direct vision to keep the distal margin clear. Excessive extrusion of the tumor may also lead to intra-operative rectal perforation, resulting in local recurrence. Thirdly, PTCT should be performed in patients with normal anal function.
In conclusion, PTCR is a procedure with a concept of organ preservation. This procedure showed clean distal margin and satisfied anal function without compromising oncological outcomes in selected patients with very low rectal cancer.
Acknowledgments
Funding: This research is supported by Project of National Key Clinical Disciplines Construction [2016].
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.10.11). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rullier E, Laurent C, Bretagnol F, et al. Sphincter-saving resection for all rectal carcinomas: the end of the 2-cm distal rule. Ann Surg 2005;241:465-9. [Crossref] [PubMed]
- Marks GJ, Marks JH, Mohiuddin M, et al. Radical Sphincter preservation surgery with coloanal anastomosis following high-dose external irradiation for the very low lying rectal cancer. Recent Results Cancer Res 1998;146:161-74. [Crossref] [PubMed]
- Schiessel R, Karner-Hanusch J, Herbst F, et al. Intersphincteric resection for low rectal tumours. Br J Surg 1994;81:1376-8. [Crossref] [PubMed]
- Martin ST, Heneghan HM, Winter DC. Systematic review of outcomes after intersphincteric resection for low rectal cancer. Br J Surg 2012;99:603-12. [Crossref] [PubMed]
- Fujii S, Yamamoto S, Ito M, et al. Short-term outcomes of laparoscopic intersphincteric resection from a phase II trial to evaluate laparoscopic surgery for stage 0/I rectal cancer: Japan Society of Laparoscopic Colorectal Surgery Lap RC. Surg Endosc 2012;26:3067-76. [Crossref] [PubMed]
- Digennaro R, Tondo M, Cuccia F, et al. Coloanal anastomosis or abdominoperineal resection for very low rectal cancer: what will benefit, the surgeon's pride or the patient's quality of life? Int J Colorectal Dis 2013;28:949-57. [Crossref] [PubMed]
- Dumont F, Ayadi M, Goéré D, et al. Comparison of fecal continence and quality of life between intersphincteric resection and abdominoperineal resection plus perineal colostomy for ultra-low rectal cancer. J Surg Oncol 2013;108:225-9. [Crossref] [PubMed]
- Konanz J, Herrle F, Weiss C, et al. Quality of life of patients after low anterior, intersphincteric, and abdominoperineal resection for rectal cancer--a matched-pair analysis. Int J Colorectal Dis 2013;28:679-88. [Crossref] [PubMed]
- Rullier E, Denost Q, Vendrely V, et al. Low rectal cancer: classification and standardization of surgery. Dis Colon Rectum 2013;56:560-7. [Crossref] [PubMed]
- Lujan J, Valero G, Biondo S, et al. Laparoscopic versus open surgery for rectal cancer: results of a prospective multicentre analysis of 4,970 patients. Surg Endosc 2013;27:295-302. [Crossref] [PubMed]
- van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210-8. [Crossref] [PubMed]
- van Gijn W, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 2011;12:575-82. [Crossref] [PubMed]
- Lee LH. Clinical and non-clinical factors influencing postoperative health-related quality of life in patients with colorectal cancer (Br J Surg 2008; 95: 1408-1415). Br J Surg 2009;96:221-author reply 221-2. [PubMed]
- Konanz J, Herrle F, Weiss C, et al. Quality of life of patients after low anterior, intersphincteric, and abdominoperineal resection for rectal cancer--a matched-pair analysis. Int J Colorectal Dis 2013;28:679-88. [Crossref] [PubMed]
- Liang JT, Cheng JC, Huang KC, et al. Comparison of tumor recurrence between laparoscopic total mesorectal excision with sphincter preservation and laparoscopic abdominoperineal resection for low rectal cancer. Surg Endosc 2013;27:3452-64. [Crossref] [PubMed]
Cite this article as: Lou Z, Gong H, He J, Zhu X, Meng R, Zhang W. Pull-through and conformal resection for very low rectal cancer: a more satisfactory technique for anal function after sphincter preserving operation. Ann Laparosc Endosc Surg 2016;1:24.


