
Operational approaches for laparoscopic complete mesocolic excision in right hemicolon cancer
In 2009, Hohenberger, a German scholar, proposed the term of complete mesocolic excision (CME), whose basic theory is mainly composed of two concepts in fetal anatomy and surgical oncology: sharp dissection of the mesocolic plane and the parietal plane. CME helps to keep the colonic mesentery intact, clarify the dissected area from central lymph nodes, emphasize the importance of transecting colon-feeding blood at the root, and increase the range of longitudinal enterotomy. Thus, CME provides a standardization of surgeries for colon cancer. Research has shown that the rate of lymph node metastasis from colon cancer ranges 5–11% (it was 6.5% among Dukes C2 cases in the MRC CLASICC trial). Therefore, central lymph node dissection is necessary. CME can maximize the clearing of the micrometastases sized <2 mm after special staining of the lymph nodes and the free tumor cells or clusters inside the lymph nodes. One tumor specimen may have 1–5 micrometastases, which may explain why CME can prolong the survival of patients with stage II colon cancer. In a prospective non-randomized trial, Galizia et al. compared the outcomes of patients who had received CME for right hemicolon cancer (n=45) or conventional right hemicolectomy (n=58). It was found that there was no local relapse in the CME group, along with significantly decreased tumor-related death. Therefore, CME is safe and feasible for right hemicolon cancer; it can remarkably reduce local relapse and increase survival rate. In particular, CME can confer long-term survival benefit in patients with lymph node-positive disease. Thus, CME reduces local recurrence rate, improves the prognosis of colon cancer, and therefore is expected to become a standard surgical procedure for the radical resection of colon cancer. Unfortunately, no randomized controlled trial (RCT) has demonstrated that CME can improve the long-term efficacy in colon cancer patients.
CME is performed via two surgical accesses: lateral access and medial access. The conventional celiotomy typically applies the lateral access. According to the previous studies performed by our group, laparoscopic CME via the medial access is comparable to traditional open colectomy. In accordance with the theory of comparative anatomy, the intermesenteric space (IMS) is located between the posterior layer of the greater omentum and the top of the transverse mesocolon and communicates only with the transverse retrocolic space (TRCS) behind the root of the transverse mesocolon; thus, the mobilization of transverse mesocolon requires the entrance of the IMS. We proposed two approaches for medial-access CME: hybrid medial approach (HMA) and complete medial approach (CMA). HMA requires the entrance of IMS via an incision of the gastrocolonic ligament, followed by the dissection of the middle colic vessels and the Henle trunk in a top-to-bottom fashion. The dissection for the inferior edge of the pancreas requires the blending of both top-to-bottom and bottom-to-top approaches. Meanwhile, CMA enters the IMS in bottom-to-top fashion, with the extension of TRCS. The approach is capped by dissection at the inferior edge of the pancreas, requiring the blending of both top-to-bottom and bottom-to-top approaches (Figure 1).
Surgical methods
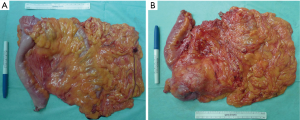
HMA
Similar to TME, the visceral fascia surrounds the whole colonic mesentery just like an envelope. During the surgery, a HIFU was used for the sharp dissection of visceral fascia and parietal fascia; the colonic mesentery was completely resected to achieve more thorough lymph node dissection and ligation of the vascular root. The West grading system was applied for evaluating the surgical quality: (I) grade A (at the layer of muscularis propria): only a small proportion of colonic mesentery is resected, with the axial nearest resection margin reaching the muscularis propria of the intestinal wall; (II) grade B (at the inner layer of colonic mesentery): parts of the colonic mesentery was irregularly resected, with the axial nearest resection margin exceeding the muscularis propria of the intestinal wall; and (III) grade C (at the layer of colonic mesentery): the colonic mesentery was completely resected, the mesenteric visceral layer was intact and smooth, and high ligation of the feeding vessels was performed.
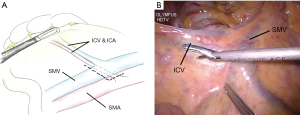
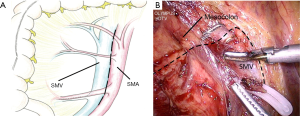
Initiation
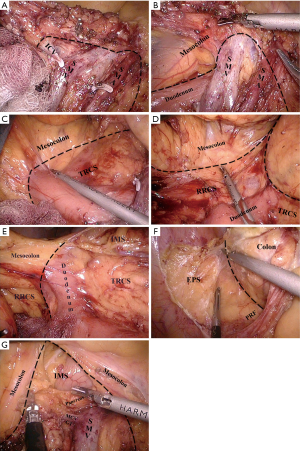
The medial approach was applied, with the projection area of ileocolic vessels (ICA and ICV) as the initiation; the vessels were dissected mainly along the superior mesenteric vein (SMV) (Figures 2 and 3).
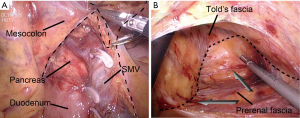
Identification and maintenance of the surgical planes
The natural surgical planes (located between Told’s fascia and anterior renal fascia) was entered to expose the head of pancreas; after the duodenum was thoroughly dissociated, the dissection continued along the lateral side till the colonic side and then turned upwards till the root of the transverse mesocolon (Figure 4). Colonic feeding vessels were dissected at their roots, and then the whole colonic mesentery was completely resected (Figure 4).
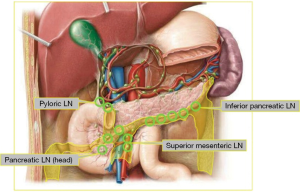
Key points of lymph node dissection
The cecum cancer and ascending colon cancer, lymph nodes on ileum-colon, right colon, and middle colic artery must be completely removed. If the cancer is at the hepatic flexure end of the transverse colon, the right gastroepiploic vein should be transected at its root for the dissection of the station 6 lymph nodes; in addition, the gastric omentum near the greater curvature of the stomach 10–15 cm away from the tumor should be removed along the gastroepiploic vessel arch (Figure 5). If necessary, the duodenum, pancreatic head, and mesenteric root should be mobilized via the Kocher approach, followed by the sharp dissection of the colonic mesentery till the superior mesenteric artery (SMA), so as to thoroughly expose the vessels feeding the colon and dissect the lymph nodes.
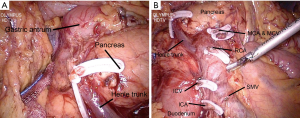
Features of the HMA
The IMS is entered via an incision of the gastrocolonic ligament, followed by the dissection of the middle colic vessels and the Henle trunk in a top-to-bottom fashion. The approach is capped by dissection at the inferior edge of the pancreas, requiring the blending of both top-to-bottom and bottom-to-top approaches.
Completely medial approach (CMA)
The CMA should also follow the principles of CME and central artery ligation.
Features of CMA
The dissection starts at the ileocolic vessel and proceeds along the SMV to enter the TRCS in bottom-to-top fashion. The dissection of the TRCS is extended laterally to the right retrocolic space (RRCS) and superiorly enters the IMS, followed by the dissection of middle colon vessels, the Henle trunk, and pancreatic lower edge in a bottom-to-top fashion (Figure 6).
Discussion
Anatomical basis of the CMA for CME
Lateral access is applied for open CME, during which the right colon was dissociated inwards firstly; then, the visceral fascia that covers the pancreas and the mesentery and the parietal peritoneum that covers the retroperitoneal tissues were sharply mobilized till the SMA to expose the colon-feeding vessels. In contrast, the laparoscopic CME applies a medial approach, during which the lymph nodes on surgical trunk were dissected firstly, followed by ligation of the central vessels, so as to achieve the mobilization of colonic mesentery outwards and upwards. The mobilization of the right hemicolon is based on one surgical plane and three avascular potential surgical spaces between intestinal canal and its nearby structure. Prerenal fascia (PRF) provides a smooth surgical plane for the mobilization of right colonic mesentery, whereas the IMSs between RRCS, TRCS, and greater omentum and the transverse mesocolon are the three surgical spaces. IMS is located between the posterior layer of the greater omentum and the top of the transverse mesocolon and communicates only with TRCS behind the root of the transverse mesocolon; thus, the mobilization of transverse mesocolon requires the entrance of the IMS (Figure 7).
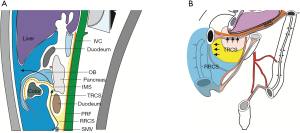
The transverse mesocolon can be completely resected after the IMS is entered by directly extending TRCS towards its head, which is the anatomical basis for CMA. The mobilization of colonic mesentery upwards can be smoothly performed via this approach; theoretically, it is more in line with the principle of CME (Figure 8). Meanwhile, it avoids the repeated turnover of the bowel and its mesentery upwards and downwards, which is required during HMA and thus can not meet the requirements of CME due to different anatomy of the upper and lower levels. Furthermore, when this approach is applied for dissection of lymph nodes at the inferior edge of pancreas, the small vessel branches at the inferior edge of pancreas can be handled under direct vision, with less bleeding. As shown in our current study, CMA can shorten the vessel ligation time, laparoscopic operative time and reduce the vascular complications, especially pancreaticoduodenal vascular complications. Therefore, CMA is a better choice for laparoscopic CME in right hemicolon cancer.
Key points and difficulties in the CMA for CME
Identification and extension of TRCS
TRCS is located between the transverse mesocolon and the inferior portion of pancreas-duodenum, with its tail connecting with RRCS at the inferior edge of the horizontal part of duodenum and its head with IMS at the root of transverse mesocolon. Therefore, proper identification and extension of TRCS is a key step in performing CMA for CME. Two ways may be applied for the proper identification of TRCS: (I) SMV is the boundary between ascending mesocolon and mesentery of small intestine and also the middle boundary of the centerline and approach of the TRCS; therefore, successful entrance to the TRCS can be achieved after sharp lateral dissection of the ascending mesocolon along the surface of the SMV sheath; (II) after the ileocolic vessels are identified, the lower portion of the SRRC can be smoothly entered and then extended upwards; then, the TRCS is entered after the mobilization of the duodenal third portion and ventral part of the pancreas. Then, IMS is entered after extension towards the head side and RRCS is entered after right extensions, so as to smoothly dissociate the colonic mesentery.
“Climbing” along the inferior edge of pancreas
During the performing of CMA, the TRCS needs to be extended upwards, IMS should be entered via the root of transverse mesocolon, and identification and “climbing” of the lower edge of pancreas is one of the key steps. Entering the posterior side of pancreas and injuring the pancreatic parenchyma, which may lead to bleeding and other vascular complications, are the potential risk of CMA. Therefore, it is particularly critical to correctly identify the lower edge of pancreas and properly grasp the timing of “climbing”. According to our experiences, after the lymph nodes on surgical trunk are dissected. The appearance of Henle trunk prompts that it is very close to the inferior edge of pancreas; dissection should then be performed forwards and upwards and “climbing” should be prepared. The appearance of right gastroepiploic vein prompts that it is time for entering IMS; dissection can be performed along the left edge of this vein, which allows easy entering of the IMS.
CME provides rational for the radical resection of right hemicolon cancer from the perspectives of fetal anatomy and surgical oncology. TMA for laparoscopic CME is technically feasible; however, it should be based on the deeper understanding of the laparoscopic anatomical plane of right hemicolon and the surgical spaces and on the fine anatomic basis. TMA for the right hemicolon CME can further shorten operative time and decrease the vascular complications and thus warrants further clinical applications.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.10.03). Ma J serves as the Managing Editor of Annals of Laparoscopic and Endoscopic Surgery. Zheng M serves as the Editor-in-Chief of Annals of Laparoscopic and Endoscopic Surgery. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Feng B, Zhang S, Yan X, Ma J, Sun J, Lu J, Li J, Wang M, Zang L, Dong F, Lu A, Zheng M. Operational approaches for laparoscopic complete mesocolic excision in right hemicolon cancer. Ann Laparosc Endosc Surg 2016;1:26.


