The future of laparoscopic major liver resection
Introduction
In the Louisville consensus meeting, laparoscopic live resection was still in its infancy and far from popularity (1). A lot of technical advancement and experience were gained during the past years, allowing surgeons to do more complex surgery. The possibility of doing laparoscopic major liver resection increased with the development of high-definition camera and display unit and a better understanding of the use of pneumoperitoneal pressure and other energy devices. In the Morioka consensus meeting, evidence of the benefits of laparoscopic liver resection started to emerge, and it was suggested that laparoscopic major liver resection should be considered as a surgical advancement worth validation and development (2).
The number of laparoscopic hepatectomies performed worldwide was exponentially increasing in the recent 2 years. Laparoscopic major liver resection has become an accepted practice, particularly for patients without cirrhosis and T2 tumor (3-9).
Technical considerations in laparoscopic major liver resection
One of the doubts about laparoscopic major liver resection is its ability to reproduce the fine and meticulous dissection done in open liver resection. Is the surgeon capable of performing anatomical liver resection with full exposure of hepatic veins?
The answer is an obvious yes nowadays. Crystal-clear high-definition videos of the procedure are often exhibited in conferences, and there are various web-based educational systems.
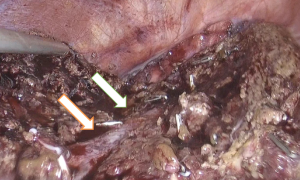
Figure 1 shows the clear exposure of the middle hepatic vein in a case of central hepatectomy.
To ensure safe practice of laparoscopic major liver resection, the surgical principle of liver resection has to be respected.
The selection criteria for laparoscopic liver resection follow exactly the same principle used for open surgery. For inclusion, liver resection has to be anatomically feasible, and there should be absence of extrahepatic disease and absence of tumor thrombosis in the main portal vein or the inferior vena cava. Patients should undergo strict preoperative liver function assessment, which includes blood test, volumetry assessment, clinical assessment and indocyanine green evaluation (10).
Meticulous anesthesia should be carried out. To prevent venous oozing from liver parenchymal transection, careful intravenous fluid administration and meticulous central venous pressure control are required. With the help of vasodilators and diuretics, the anesthesiologist should cautiously keep the central venous pressure at preferably below 5 cmH2O.
In major liver resection, the portal pedicle is dissected clearly from the Glisson capsule. The portal vein, hepatic artery and bile duct are separately controlled and divided. The patient is usually placed in the Lloyd-Davis position. The primary surgeon stands between the legs with one assistant on each side. Pneumoperitoneum is usually done by subumbilical incision. Three to four working ports measuring from 5 to 12 mm are used. This allows the use of an ultrasonic dissector or a CUSA for parenchymal transection (10,11).
Pringle maneuver can be applied when necessary. The pneumoperitoneal pressure can be elevated up to 18 mmHg to reduce venous oozing when needed.
With vigilant dissection under optimized pneumoperitoneal pressure, the hepatic vein can be fully exposed without bleeding.
Evidence of benefits of laparoscopic major hepatectomy
In 2011, there was very weak evidence that laparoscopic major liver resection was an accepted method for cancer treatment because the operation time was longer while the amount of blood loss was not less, and there were no long-term data of oncological outcomes (12). The data in 2011 were actually a reflection of accumulation of experience in major hepatectomy between 2005 and 2010. The experience at that time was still experimental and surgeons were struggling with low-definition cameras and basic laparoscopic instruments.
Evidence favoring laparoscopic major liver resection became stronger in 2016. More than 1984 cases of laparoscopic major hepatectomy have been performed worldwide (13).
Table 1 is a summary of outcomes of laparoscopic major hepatectomy reported by various studies (4-9). We can see that there is a consistency in reduction of overall complications, blood loss and hospital stay. However, up to this moment, operation time is still more or less the same. Laparoscopic major hepatectomy is a complex surgery and there is still plenty to learn.
Table 1
| Authors | Year | No. of patients | Open liver resection | Laparoscopic major liver resection | Blood loss | Operation time |
|---|---|---|---|---|---|---|
| Yoon et al. | 2016 | 152 | 115 | 37 | 136 vs. 110 mL, P=0.856 | 200 vs. 304 min, P<0.0001 |
| Medbery et al. | 2014 | 115 | 48 | 67 | 737 vs. 281 mL, P=0.002 | 285 vs. 233 min, P<0.001 |
| Abu et al. | 2013 | 84 | 46 | 38 | 435 vs. 100 mL, P<0.001 | 150 vs. 145 min, P=0.021 |
| Topal et al. | 2012 | 40 | 20 | 20 | 550 vs. 550 mL, P=0.884 | 233 vs. 258 min, P=0.228 |
| Martin et al. | 2010 | 450 | 360 | 90 | 400 vs. 150 mL, P<0.0001 | 160 vs. 150 min, P=0.009 |
| Cai et al. | 2009 | 38 | 19 | 19 | 895 vs. 462 mL, P=0.516 | 204 vs. 222 min, P=0.516 |
The oncological outcomes of laparoscopic major hepatectomy still need to be validated, but some initial results showed that the oncological outcomes of laparoscopic major hepatectomy were not inferior to those of open liver resection.
Learning laparoscopic major liver resection
Before doing laparoscopic major liver resection, a surgeon should have adequate experience in open hepatectomy and minor liver resection.
Understanding the difficulty score for laparoscopic liver resection is crucial for case selection. The operation can be carried out safely only when the surgeon’s experience level matches the difficulty score. The scoring system was developed as a pre-conference task before the 2nd International Consensus Conference on Laparoscopic Liver Resection 2014 in Morioka, Japan (2).
The scoring system consists of five factors from preoperative information forming the basis of difficulty levels: (I) tumor location; (II) extent of liver resection; (III) tumor size; (IV) proximity to major vessels; and (V) liver function. This difficulty index is comprised of the cumulative score for the five individual factors (2,14,15).
A score of 1–3 means that surgery with low complexity is required, which is ideal for surgeons starting to do laparoscopic liver resection. A score of 4–6 means that surgery with intermediate complexity is required, which should be performed by surgeons who can consistently perform laparoscopic liver resection in low-difficulty cases. A score of 7–10 means that surgery with high complexity is required, which should only be performed by surgeons with ample experience in laparoscopic hepatectomy.
It is important to possess ample experience in laparoscopic minor liver resection before learning to do laparoscopic major liver resection.
In a study of 173 laparoscopic liver resections, Nomi et al. concluded that an experience of 45–75 cases is required for a surgeon to overcome all the difficulties in major liver resection. In a study of 159 laparoscopic liver resections, Poel et al. concluded that an accumulation of 55 cases is necessary in order to reduce the incidence of conversion and complication.
Conclusions
Laparoscopic major hepatectomy remains a complex operation in the field of hepatobiliary and pancreatic surgery. Although the current evidence of its benefits is small when compared with that of open surgery, the number of laparoscopic surgery is exponentially increasing, and there is a lag time of 2–3 years for publication. More and more centers are doing laparoscopic major liver resection safely.
The future is now.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Giovanni Battista Levi Sandri) for the series “Laparoscopic Liver Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.01.02). The series “Laparoscopic Liver Surgery” was commissioned by the editorial office without any funding or sponsorship. TTC serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Jul 2016 to Jun 2018. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Cheung TT, Dai WC, Tsang SH, et al. Pure Laparoscopic Hepatectomy Versus Open Hepatectomy for Hepatocellular Carcinoma in 110 Patients With Liver Cirrhosis: A Propensity Analysis at a Single Center. Ann Surg 2016;264:612-20. [Crossref] [PubMed]
- Yoon YI, Kim KH, Kang SH, et al. Pure Laparoscopic Versus Open Right Hepatectomy for Hepatocellular Carcinoma in Patients With Cirrhosis: A Propensity Score Matched Analysis. Ann Surg 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Abu Hilal M, Di Fabio F, Syed S, et al. Assessment of the financial implications for laparoscopic liver surgery: a single-centre UK cost analysis for minor and major hepatectomy. Surg Endosc 2013;27:2542-50. [Crossref] [PubMed]
- Cai XJ, Wang YF, Liang YL, et al. Laparoscopic left hemihepatectomy: a safety and feasibility study of 19 cases. Surg Endosc 2009;23:2556-62. [Crossref] [PubMed]
- Martin RC, Scoggins CR, McMasters KM. Laparoscopic hepatic lobectomy: advantages of a minimally invasive approach. J Am Coll Surg 2010;210:627-34, 634-6.
- Topal H, Tiek J, Aerts R, et al. Outcome of laparoscopic major liver resection for colorectal metastases. Surg Endosc 2012;26:2451-5. [Crossref] [PubMed]
- Medbery RL, Chadid TS, Sweeney JF, et al. Laparoscopic vs open right hepatectomy: a value-based analysis. J Am Coll Surg 2014;218:929-39. [Crossref] [PubMed]
- Cheung TT, Poon RT, Yuen WK, et al. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 2013;257:506-11. [Crossref] [PubMed]
- Cheung TT, Poon RT. Synchronous resections of primary colorectal tumor and liver metastasis by laparoscopic approach. World J Hepatol 2013;5:298-301. [PubMed]
- Nguyen KT, Marsh JW, Tsung A, et al. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg 2011;146:348-56. [Crossref] [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Ban D, Tanabe M, Ito H, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 2014;21:745-53. [Crossref] [PubMed]
- Ban D, Kudo A, Ito H, et al. The difficulty of laparoscopic liver resection. Updates Surg 2015;67:123-8. [Crossref] [PubMed]
Cite this article as: Cheung TT. The future of laparoscopic major liver resection. Ann Laparosc Endosc Surg 2017;2:13.