The technical characteristics and clinical analysis of laparoscopic bursectomy for advanced gastric cancer
Introduction
Whether patients with advanced gastric carcinoma should receive bursectomy or not has existed for a long time (1-4). There are anatomical, physiopathological and clinical practice reasons for this: (I) anatomically speaking, bursa omentalis (5) is constituted by anterior lobe of transverse mesocolon, pancreatic capsule, greater momentum, lymph connective tissue of hepatoduodenal ligament, hepatogastric ligament, phrenogastric ligament, hepaticopancreatic fold and gastropancreatic fold. These are all originated from the same embryonic layer. There are gastric vessel branches, lymphatic vessels, lymph nodes, fat, fascia and so on inside these ligaments, folds and perigastric mesogastriums. On the other hand, outside bursa omentalis there are fascias and intrafascial space and there are no vessels and lymphatic vessels in it. So to speak, the safe dissective planes in gastric surgery, should be subjected to outside bursa omentalis along the fascias and intrafascial space to achieve an en bloc resection of bursa omentalis, lymph nodes, gastric tissue and so on. (II) Physiopathologically speaking, perigastric mesogastriums and fusion fascia is barrier to keep cancer cells from spreading and metastases. But, it is likely for gastric cancer cells invasion and lymph node metastasis in fascias and intrafascial space between the perigastric mesogastriums and perigastric organs (6). Also gastric cancer cell metastasis occurs on the pancreatic capsule and anterior lobe of transverse mesocolon through lymphatic vessels which connect bursa omentalis and gastric serosal. For these patients with posterior gastric wall trans-serosal cancer, exfoliative cancer cells always colonize in the bursa omentalis. Therefore, an en-bloc removal of free cancer cells, micrometastases and lymphatic metastases contained in the bursa omentalis, is potential surgical procedure in radical gastrectomy. (III) Clinically speaking, exfoliative cancer cells, cancer cells inside the vessels and lymphatic ducts may flow into the abdominal cavity with blood and lymphatic fluid during operation, this is the important factor of postoperative intraperitoneal recurrence (3).
Furthermore, the Japanese Classification of Gastric Carcinoma (the 14th edition) also suggests that patients with gastric posterior wall sensor invaded (T3–T4a) should receive bursa omentalis resection in order to clean up the micrometastasis in bursa omentalis. In Japan, Korea and China, bursectomy and D2 lymphadenectomy are regarded as a standard surgical procedure during radical open gastrectomy for serosa-positive gastric cancer. It has been reported that bursectomy could prevent cancer cells scattered and removed peritoneal micro-metastasis (7,8) but there is much difficulty performing bursectomy in radical operation for gastric cancer of laparoscopy. Currently, some surgeons of Japan, Korea and China try to perform laparoscopic resection of pancreatic capsule and anterior transverse mesocolon.
Based on our previous experience of more than 300 cases laparoscopic surgery for gastric cancer every year in our medical center and the clinical research of laparoscopic bursectomy (9,10), we analyze technical characteristics and clinical experience of laparoscopic bursectomy for advanced gastric cancer.
Patient selection and workup
The patient selection and workup are: (I) patients were diagnosed with advanced gastric cancer without metastasis; (II) CT and endoscopic biopsy diagnosed; (III) TNM staging is T3–T4a; (IV) patients agree with surgery and sign the consent form.
Pre-operative preparation
The pre-operative preparation is same as the general abdominal surgery, ruled out surgery contraindications.
Equipment preference card
The equipment preference card is same as the laparoscopic gastrectomy.
Ethics
Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine Hospital approved this study. The information of patients was written consent to be stored in the hospital database and used for research.
Procedures
Laparoscopic bursectomy (LP) is highly technically demanding, the surgeon and its team should be skilled and experienced in open bursa omentalis resection and have well-knit basic skills in using laparoscope. It is better that the surgeons who had previously completed more than 100 cases of laparoscopic radical gastrectomy for gastric cancer. The detailed operation steps are as follows.
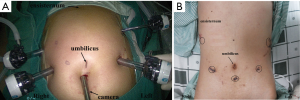
Trocar and operator’s position
Patients were placed in the reverse Trendelenburg position and the location of the Trocar adopts five-hole method. First the surgeon stands on the right side, and then in the middle of the legs of the patients (Figure 1).
Main steps
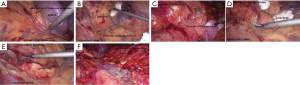
Step one
Triangle pull the greater momentum on the right side of transverse colon, dissect the clearance between the transverse mesocolon and distal gastric membrane from right to left with the No.6 LNs dissection, enter the duodenal posterior clearance to dissect the capsule of pancreas and the anterior lobe of transverse mesocolon from right to left (Figure 2).
Step two
Enter the anterior space of pancreas with dissect the capsule of the pancreas and the anterior lobe of transverse mesocolon from left to right, converge the separated panes from right to left. To this moment, the pancreas capsule and the anterior plane of transverse mesocolon were completely separated outside bursa omentalis (Figure 3).
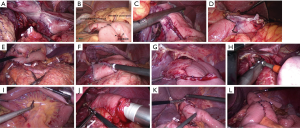
Step three
For radical distal gastrectomy, enter the posterior of stomach with the No. 4, No. 7, No. 9 and the No. 8 LNs. For radical total gastrectomy, outside bursa omentalis to enter the posterior of stomach and splenic hilar with No. 11d, No. 10 and No. 1 LNs dissection with spleen-preserving, mobilizing the left side of abdominal esophagus (Figure 4).
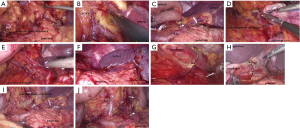
Step four
Expose the right lateral of bursa omentalis with the No. 5, No. 12 LNs dissection, transect the duodenum with linear cutter and dissect the No. 8, No. 9, No. 7, No. 11p LNs under the assistant’s Triangle pull the distal end of the stomach to the left outside bursa omentalis, separate right abdominal esophagus with the No. 3 and No. 1 LNs dissection (Figure 5). At this point, for radical total gastrectomy, bursectomy and D2 lymphadenectomy were completed. Surgeon reconstructs the digestive tract under laparoscopy with Billroth II or Billroth I for distal radical gastric resection, Roux-en-Y esophagus jejunum anastomosis for radical total gastric resection (Figure 6).
Role of team members
Liao-Nan Zou, GI surgeon, MD:
- A member of China South Cooperation Team of Laparoscopic Colon Surgery.
- A member of the Institute of Clinical Research of Sun Yat-Sen University.
- A member of the Editorial Board Certificate of Journal of Laparoscopic Surgery.
- A member of Upper Gastrointestinal Surgeon Committee of China Medical Doctor Association.
- A member of Anal Rectal Physicians Committee of China Medical Doctor Association.
- Peer-reviewer of Chinese Journal of Colorectal Disease (Electronic Edition).
- Peer-reviewer of Disease of Colon &Rectum (DCR).
Jin Wan, GI surgeon, PhD:
- Vice Chairman of the Colon Cancer Committee of the Guangdong Province Anti-cancer Association.
- Vice Chairman of the Minimally Invasive Surgery of the Guangdong Province Medical Doctor Association.
Post-operative management
Helping patients get out of bed to take physical activities from the first day after the operation; stop gastrointestinal decompression after the first postoperative flatus, giving fluid diet in order to make transition from parenteral nutrition (PN) to enteral nutrition (EN).
Tips, tricks and pitfalls
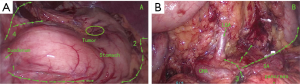
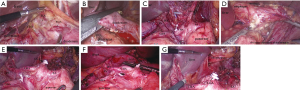
Approach for the procedure (bursectomy)
During the whole procedures, dissect around the pancreas as it serves as the main anatomical landmark. Dissecting the anterior lobe of transverse mesocolon and the Pancreatic Capsule on both flank (first from their right and then from their left), it makes easy to dissect according to the characteristics of its anatomical features. Dissect from the greater curvature of the stomach to the lesser curvature of the stomach, from the distal to the proximal stomach, bursectomy and dissection of lymph nodes at the same time. Distal stomach (Figure 7).
Tips, tricks and pitfalls for surgical exposure and dissection
During the procedure, surgical exposure is very important for the dissection. Besides the Hang liver, the triangle pull by the surgeon and the assistant is applied all through the procedure. It makes it easier to dissect the bursa omentalis and lymph nodes. Sometimes, the surgeon dissect with pulling by a gauze, this is not only to expose but also not to break the bursa omentalis, especially for dissecting the anterior lobe of transverse mesocolon and the pancreatic capsule (Figure 8A-C).
In the first step, the completion of the No. 6 LN dissection makes it easy to dissect the head of the pancreatic capsule. Entering the right anatomical structure is a key step to begin the procedure and maintain bursa omentalis’s integrity.
In the second step, it is liable to enter the posterior of the pancreatic space when dissecting the capsule of the tail of pancreas (the red line is the right approach to dissect (Figure 8D).
Outside bursa omentalis enter the gastric posterior space and mobilize the splenic hilar posterior. This makes it easy for laparoscopic spleen-preserving splenic hilar lymph node dissection for radical total gastrectomy for proximal gastric cancer.
Overall, the procedure should carry out in the fascial space outside bursa omentalis, using the combination of sharp and blunt dissection. Generally speaking, complete bursectomy will not achieved without total radical gastrectomy, because the complete resection of the bursa omentalis including not only the capsule of pancreas and the anterior lobe of transverse mesocolon, but also the greater momentum, the lymph connective tissue of hepatoduodenal ligament, the hepatogastric ligament, the phrenogastric ligament, the hepatopancreatic fold, the gastropancreatic fold and the extension of the caudate lobe of the liver capsule. But we can finish the resection of the tissue mentioned above except for the extension of the caudate lobe of the liver capsule, because it is impossible to do that. Therefore, the scope of its procedure is larger than the D2 radical gastrectomy which is recommended by the guideline, besides the tissue mentioned above, the scope also includes such as the No. 8P LNs and No. 12P LNs. However, whether the resection of the bursa omentalis is completed may be decided by the patients’ physical condition and the surgeons’ skill, including the nature and amount of the case’s mesenteric fat, degree of bleeding tendency and degree of fascial porosity.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.11.17). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine Hospital (No. T2016-002-01) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011;14:113-23. [Crossref] [PubMed]
- Yoshikawa T, Tsuburaya A, Kobayashi O, et al. Is bursectomy necessary for patients with gastric cancer invading the serosa? Hepatogastroenterology 2004;51:1524-6. [PubMed]
- Yamamura Y, Ito S, Mochizuki Y, et al. Distribution of free cancer cells in the abdominal cavity suggests limitations of bursectomy as an essential component of radical surgery for gastric carcinoma. Gastric Cancer 2007;10:24-8. [Crossref] [PubMed]
- Hundahl SA. The potential value of bursectomy in operations for trans-serosal gastric adenocarcinoma. Gastric Cancer 2012;15:3-4. [Crossref] [PubMed]
- Han F, Zhan W, He Y. Radical Resection of Bursa omentalis and fascia in Gastric Carcinoma. Chin J Bases Clin General Surg 2007;14:230-4.
- Bi JW, Du CH, Wei G, et al. Resection of pancreatic capsule and anterior layer of transverse mesocolon in radical gastrectomy and its clinical significance. Zhonghua Wei Chang Wai Ke Za Zhi 2009;12:467-70. [PubMed]
- Fujita J, Kurokawa Y, Sugimoto T, et al. Survival benefit of bursectomy in patients with resectable gastric cancer: interim analysis results of a randomized controlled trial. Gastric Cancer 2012;15:42-8. [Crossref] [PubMed]
- Imamura H, Kurokawa Y, Kawada J, et al. Influence of bursectomy on operative morbidity and mortality after radical gastrectomy for gastric cancer: results of a randomized controlled trial. World J Surg 2011;35:625-30. [Crossref] [PubMed]
- Zou LN, He YB, Li HM, et al. Surgical skills for laparoscopic resection of the bursa omentalis and lymph node scavenging with radical gastrectomy. Oncol Lett 2015;10:99-102. [PubMed]
- Zou L, Xiong W, Mo D, et al. Totally laparoscopic complete bursectomy and D2 lymphadenectomy in radical total gastrectomy: an outside bursa omentalis approach. Surg Endosc 2016;30:4152. [Crossref] [PubMed]
Cite this article as: Zou LN, Zheng BS, Liu PF, Wan J. The technical characteristics and clinical analysis of laparoscopic bursectomy for advanced gastric cancer. Ann Laparosc Endosc Surg 2017;2:45.