Surgical repair in recurrent inguinal hernia
Introduction
The incidence of recurrence is most often held as the measure of success used to compare the various methods of inguinal herniorrhaphy. With 13% of all groin hernia repairs being performed for recurrent hernias, recurrence after inguinal hernia repair remains a clinical problem in present day scenario (1). The incidence of recurrence after inguinal hernia repair is difficult to estimate accurately since it varies with duration of follow-up, but may be as high as 15% (2). In a long-term Danish observational study, which was published in 2014 showed that the reoperation rate after primary Lichtenstein repair to be 2.4%, and after laparoscopic repair to be 3.3%, which has been ranging from 1–4.3% for trans-abdominal pre-peritoneal repair (TAPP) and from 0–3.5% for total extra-peritoneal repair (TEP) (3-5). All the measures to decrease the burden of recurrences should be used which can only be done by getting the knowledge of patient-related risk factors along with knowledge of the controllable technical risk factors (Table 1).
Table 1
| Technique | Tissue repair (except Shouldice) | Shouldice technique | Lichtenstein | Stoppa’stechnique | TEP | TAPP |
|---|---|---|---|---|---|---|
| Recurrence rates | 10–30% | 0.2–4.8% | 0.5–2.4% | 0–7% | 0–3.5% | 1–4.3% |
TEP, total extra-peritoneal repair; TAPP, trans-abdominal pre-peritoneal repair.
Etiological factors
A number of factors may contribute to the recurrence of an inguinal hernia. These may be classified into patient-related, surgeon-related and surgery/technique-related which are mentioned in various HerniaSurge Guidelines (6-15).
Patient-related factors
General factors
- Gender: females are more prone to inguinal hernia recurrence than males, high level of evidence is available to show that (6).
- Obesity: obesity has shown a moderate level of link with increased recurrence (6).
- Age: increased age has not been consistently associated with increased recurrence (6).
- Chronic constipation has not been consistently proven by studies but this is believed to promote recurrence (6).
- Smoking and COPD (chronic cough) although has not been consistently demonstrated in literature, but are often considered risk factors for recurrence (6).
- Liver cirrhosis has not been consistently proven to be a risk factor for recurrence (6).
- Family history: recurrence has not shown been shown to be affected by positive family history (6).
- Chronic kidney disease, social class, occupation, work load, pregnancy, labor and race are incompletely studied factors, which may impact the risk of inguinal hernia recurrence (6).
Local factors
- Type of hernia: high level of evidence shows that direct hernias are more likely to recur (6).
- Sliding hernias: sliding hernias are associated with increased recurrence has moderate level of evidence (6).
- Size of hernia: it has been shown that size of hernia, <3 versus ≥3 cm does not appear affect the risk of recurrence (6).
- Bilaterality of inguinal hernia has not shown any associated increased recurrence (6).
- Collagen levels: moderate level of evidence is available to suggest that diminished collagen type I/III ratio is associated with increased recurrence (6).
- Matrix metalloproteinase (MMP) levels: a moderate level of evidence shows that increased systemic MMP levels are associated with increased recurrence (6).
Surgeon-related factors
Less experienced and unsupervised trainees (i.e., <60 cases or 3 years’ experience), performing open anterior mesh repair, studies have shown to have higher recurrence rates and longer operative times suggesting limited technical competency (7). However, supervised and extensive experience training modifies this factor. Laparoscopic inguinal hernia repair is a technically advanced laparoscopic procedure with a steep learning curve. A varying number of cases 40–250, which has been quoted by numerous studies, are mandatory for acquiring sufficient technical expertise (8-11). The recurrence rate is seen to decline and stabilize over the first 100 cases, however, conversions, complications and operating time have been seen to improve even after 250 cases, which concludes that factors other than surgical expertise and surgeon’s competence operate in the causation of recurrences (11).
Surgical technique & surgery-related factors
Surgical technique factors
Paying attention to surgical technique and following standardized surgical steps can contribute to lower recurrence rates. This is due to the fact that incorrect operative technique is one of the most important reasons for recurrence (7).
- Sac invagination, without ligation in an indirect hernia management by open surgery, is associated with an increased incidence of recurrence (12).
- Open repairs done under tension are associated with increased recurrence. Thus tension-free mesh repair should always be done (12).
- Recurrence may increase in a case of inadequate dissection of pre-peritoneal space. An exposure of the entire myopectineal orifice is needed in laparo-endoscopic repair to ensure adequate overlap of the mesh on all potential hernia sites. In a scenario in which an inadequate dissection is done, it may result in the use of either a small mesh customized to fit the available space while on the other hand in case a larger mesh is used, the resultant mismatch between the available inadequate space and a larger mesh may predispose the mesh to fold or roll (12). Either situation predisposes to a recurrence. This occurs due to intra-abdominal shearing forces causing the folded mesh to slide away from the defect or due to migration of a small mesh into the hernia defect by forces responsible for causing the hernia. On the other hand a large mesh in a small space may balloon out through the defect giving the appearance of a recurrence.
- In case there is a presence of pre-peritoneal lipoma that is not dissected out. The lipoma acts like a pseudo-recurrence (13).
- Missed hernia: recurrences might represent hernias overlooked during primary operations which are shown by the fact that femoral hernia recurrences are found in roughly 40% of reoperations in women (14).
- Mesh choice: the effect of weight differences alone on surgical outcomes is unknown. There is no clearly defined weight limit for LWMs and HWMs (15).
- Fixation: recurrence may be associated with improper fixation technique. Tissue-mesh interface is the weakest link in a prosthetic hernia repair. Most of the times, this is the site where the repair gives way. Poor grip of the weakened tissues or avulsion of the fixation device due to pressures and strain acting on the mesh could cause give-way of the mesh. The mesh should be fixed well away from the hernia site (using fixation devices with sufficient tissue penetration to resist disruptive intra-abdominal forces) to tissues with strong inherent strength. The aim of mesh fixation is mesh fixation in large hernias is to prevent early displacement, mesh migration and a consequent recurrence. According to the HerniaSurge Guidelines, in open anterior mesh groin hernia repairs there are no differences in recurrence between different fixation methods (16). Traumatic mesh fixation is recommended in patients with large direct hernias (M3-EHS classification) undergoing TAPP or TEP to reduce recurrence risk (16).
- Mesh size, defect overlap & mesh contraction: All meshes are known to contract and shrink in size. Hence, selection of a mesh size that is too small or that provides inadequate overlap is associated with increased recurrence. However, excessive shrinkage of mesh in spite of adequate overlap may predispose to recurrence (15).
- Anaesthesia: a moderate level of evidence shows that open hernia repair under local anesthesia done by general surgeons is associated with recurrence (6). When surgeons inexperienced in its use administer local anesthesia, more hernia recurrences might result.
Surgery related factors
- Early postoperative hematoma formation is associated with increased recurrence as theoretically it may result in lifting of the mesh away from the tissues but this is not consistently demonstrated in literature (6).
- There is no conclusive study to suggest role of postoperative seromas in hernia recurrence (6).
- Emergency surgery may be a risk factor for hernia recurrence, but there is no conclusive data to support it (6).
- Surgical site infections (SSIs) are not consistently shown to be associated with recurrence (6).
- Post-operative physical activities: no evidence to show any effect on recurrence with work and leisure activities, which can be resumed by most patients within three to five days following elective laparoscopic/open inguinal hernia repair (6).
Assessment of a patient with recurrent inguinal hernia repair
It is important to have to complete detail about prior surgical history. An ideal scenario would be one in which previous operative notes were available for reference, to know about the type and size of mesh and any difficulty during previous surgery. Irrespective of the previous surgical technique, the repair of a recurrent inguinal hernia is likely to be difficult, with increased operative time and greater chance of injury. Hence it should only be undertaken by an experienced surgeon, preferably in a specialized hernia centre.
Clinical evaluation, additionally supported by ultrasound examination of the groin region is sufficient in most cases to confirm the diagnosis of recurrence. Perform the Valsalva manoeuvre during testing which will help in forcing a possibly occult or small hernia into its abnormal channel and more clearly demonstrate its presence. If still there is a diagnostic dilemma, a dynamic MRI or CT can be considered (17).
Treatment options and decision- making for surgical repair of recurrent inguinal hernia
Repair of a recurrent inguinal hernia is technically more demanding for the surgeon because of the fact that scar tissue causes the inguinal canal to be distorted. In addition there is a substantially higher risk for complications or development of another recurrence, as the tissue tends to be weaker than at the time of primary repair. Although a lot has been published about primary repair of inguinal hernias, less is known about the best approach to address a recurrent hernia. Although watchful waiting can a management option for asymptomatic or minimally symptomatic inguinal hernias, but the conventional approach is to offer all patients with a recurrence an operative management strategy. There is no evidence either for or against such a strategy in case of recurrent inguinal hernias (18).
The decision would rest on patient preference as well as surgeon choice, and is best made after a detailed discussion with the patient. In a patient who has had a previous tissue repair, without mesh implantation, are suitable candidates for both anterior (open) as well as posterior (open/endo-laparoscopic) approach (19). Although the scarring of the tissues would be less than if a mesh were used as a prosthesis, but dissection of fibrosed tissue would be required in anterior open approach and hence increase the chances of injury to various structures. Thus, in this situation the posterior approach has an edge over the anterior route, and the preferred technique would be laparo-endoscopic approach.
In cases where a previous mesh has been implanted by the open anterior route, as it is recommended in guidelines to repair the hernia via virgin tissue planes, thus a posterior approach (open/laparo-endoscopic) would be preferred (19). One would encounter heavy scarring and distorted tissue planes if attempts an anterior approach, due to the presence of a previously implanted mesh, thus increasing the risk of nerve entrapment, chronic pain and testicular atrophy. Additionally, there is earlier return to work and lower incidence of chronic groin pain associated with the laparo-endoscopic approach. However, one should be aware of the fact that, if expertise in laparo-endoscopic technique is not available, an open posterior approach is an acceptable treatment option because TEP/TAPP after previous anterior mesh repair is associated with increased peritoneal tears during surgery and longer operative times.
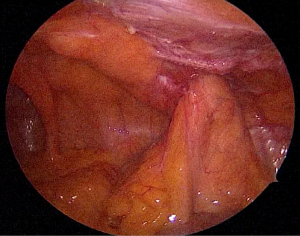
In case of recurrence after a previous endo-laparoscopic hernia repair, guidelines recommend an anterior mesh placement (18). Due to same principle as followed after open surgery recurrence, this is to avoid re-surgery in the posterior plane where previously placed mesh and fibrosis will have distorted the normal anatomy. However, there are case series and reports of the use of TAPP to treat recurrences after TEP/TAPP (Figures 1 and 2).
A difficult situation sometimes encountered is the case of the re-recurrent inguinal hernia. Such a patient has had more than one repair involving both the anterior as well as posterior planes. In this case, recommendation is to do a re-laparoscopy, either modified laparoscopic intra-peritoneal onlay mesh (IPOM) or a TAPP by an experienced laparoscopic hernia surgeon (19). Due the requirement of using a non-barrier mesh since it will come in contact with intra-abdominal viscera, the laparoscopic IPOM technique is expensive for the patient. Also, one is unable to ensure proper mesh fixation without dissection of the groin, and this may pre-dispose to re-recurrence. Other issues associated with the IPOM technique are that the sac is not dissected out and is left in situ.
Surgical principles in the repair of recurrent inguinal hernia
Based on HerniaSurge Guidelines and International Endohernia Society (IEHS) guidelines a surgeon should follow these surgical principles for better results in recurrent inguinal hernia surgery (17-21).
- The most important principle in the repair of a recurrent inguinal hernia is to approach the area through undisturbed tissue planes. That is, in case of previous anterior repair on should use the posterior route to repair the recurrence, and vice versa.
- Scarring and distortion of tissue planes is expected. One should always do a careful dissection technique in order to try and restore the normal anatomy.
- In anterior approach, reinforce the entire inguinal floor irrespective of the type of hernia and do not depend on fascial structures to close or reinforce the defect.
- Dissection should proceed from normal tissue to scarred tissue and from familiar structure to unfamiliar. Avoid use of scarred or devascularized tissue in the re-pair of recurrent hernias.
- Avoid any tension on suture lines.
- The previous mesh should not be removed. Removal of a previously implanted pre-peritoneal mesh may increase the risk for lesion of urinary bladder, bleeding complications, and substantial defects of the peritoneum. The presence of two or more meshes in the inguinal region does not seem to enhance the frequency of chronic pain.
- In recurrent inguinal hernia repair a complete dissection and exposure of the entire groin to visualize all potential sites of herniation, as “missed” femoral hernias account for a significant number of recurrences. In case of laparo-endoscopic approach, this is part of the surgical process. But an effort should be made to incorporate this step in an open repair technique.
- The mesh should be of appropriate size in order to have adequate overlap of the margins and ensure complete coverage of the defect. The new mesh should be placed over the old one in order to correct the error of previous slipped or misplaced mesh (20,21).
Contraindications
Active infection is a contraindication, as mesh should be used in virtually all repairs of a recurrent inguinal hernia.
Proposed approach for recurrences
In view of these general principles, the approach that a surgeon should follow to the repair of a recurrent inguinal hernia is proposed based upon the surgical repair technique for the primary hernia: anterior repair or posterior repair.
Anterior hernia repair failure
For patients with a failed anterior mesh repair, the procedure of choice is to use a posterior approach to the hernia repair such as a laparoscopic transabdominal preperitoneal hernia (TAPP) mesh repair or totally extraperitoneal hernia repair (TEP) or open pre-peritoneal approach.
In a retrospective study done by Sevonius et al. based on Swedish hernia register, a review of 19,582 operations for a recurrent hernia were done, compared with other techniques, the laparoscopic and open pre-peritoneal approaches were significantly associated with the lowest rate of subsequent recurrences of 1.4% (22).
Posterior hernia repair failure
In patients who have undergone a prior posterior hernia repair such as a laparoscopic hernia repair, the preferred technique is based on surgeons experience with laparoscopic hernia repair surgeries. In cases where surgeon is not experienced for complex and difficult hernia repair surgeries via laparoscopic approach, tension-free anterior approach such as a Lichtenstein mesh repair is preferred approach. This allows the surgeon to operate in mostly undisturbed planes, facilitating identification of the hernia defect. If the recurrence is a femoral hernia, the preferred technique in this setting is either an infra-inguinal mesh plug repair or a modified Lichtenstein repair with the inferior edge of the mesh fastened to Cooper’s ligament.
The major advantage in laparo-endoscopic repair is when the exact location of the recurrent hernia is unclear, a laparoscopic approach offers access to all potential sites of recurrent hernia (e.g., direct, indirect and femoral). Laparo-endoscopic repair approach can be taken by experienced laparoscopic surgeon keeping in mind that dissection of the preperitoneal plane is often difficult after a previous posterior mesh repair. For that reason, an attempt at a repeat TEP will often result in a peritoneal breach, forcing conversion to a TAPP. Therefore, any surgeon who is attempting a laparoscopic re-repair of a recurrent hernia after a prior preperitoneal repair must be comfortable with both TEP and TAPP techniques.
Meta-analysis studies
Two meta-analysis studies were done for patients with recurrent inguinal hernias which evaluated the recurrence rate and morbidities for laparoscopic and open repairs (23,24).
Results showed that patients treated with a laparoscopic repair had significantly less pain, fewer superficial wound infections, longer operative times, shorter length of time to return to daily activities, significantly fewer hematomas and seromas with laparoscopic repair. No significant difference in early and overall recurrence rate.
Conclusions
Inguinal hernia repair is one of the most frequently performed elective operations today. Recurrence after inguinal hernia surgery remains a clinical problem. The incidence of recurrence after inguinal hernia repair is difficult to estimate accurately since it varies with duration of follow-up, but may be as high as 15%. All the measures to decrease the burden of recurrences should be used which can only be done by getting the knowledge of patient-related risk factors along with knowledge of the controllable technical risk factors. It is important to have to complete detail about prior surgical history. Surgeon should follow certain principles and guidelines for operating a recurrent inguinal hernia. The decision would rest on patient preference as well as surgeon choice, and is best made after a detailed discussion with the patient.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery for the series “Inguinal Hernia Repair”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.05.03). The series “Inguinal Hernia Repair” was commissioned by the editorial office without any funding or sponsorship. Sharma A served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study did not require any approval by institutional ethical committee or informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kehlet H, Bay-Nielsen M. Nationwide quality improvement of groin hernia repair from the Danish Hernia Database of 87,840 patients from 1998 to 2005. Hernia 2008;12:1-7. [Crossref] [PubMed]
- Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 2004;350:1819-27. [Crossref] [PubMed]
- Burcharth J, Andresen K, Pommergaard HC, et al. Recurrence patterns of direct and indirect inguinal hernias in a nationwide population in Denmark. Surgery 2014;155:173-7. [Crossref] [PubMed]
- Burcharth J. The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J 2014;61:B4846. [PubMed]
- Eklund AS, Montgomery AK, Rasmussen IC, et al. Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair – A randomized, multicenter trial with 5 year follow-up. Ann Surg 2009;249:33-8. [Crossref] [PubMed]
- Jorgensen LN, Hope WW, Bisgaard T. Risk Factors for the Development of Inguinal Hernias in Adults. Chapter 2. HerniaSurge Guidelines Part 1. Available online: www.herniasurge.com
- Bingener J, Simmermacher R, Lomanto D, et al. Training and the Learning Curve. Chapter 22. HerniaSurge Guidelines Part 3. Available online: www.herniasurge.com
- Bansal VK, Krishna A, Misra MC, et al. Learning Curve in Laparoscopic Inguinal Hernia Repair: Experience at a Tertiary Care Centre. Indian J Surg 2016;78:197-202. [Crossref] [PubMed]
- Lim JW, Lee JY, Lee SE, et al. The learning curve for laparoscopic totally extraperitoneal herniorrhaphy by moving average. J Korean Surg Soc 2012;83:92-6. [Crossref] [PubMed]
- Choi YY, Kim Z, Hur KY. Learning curve for laparoscopic totally extraperitoneal repair of inguinal hernia. Can J Surg 2012;55:33-6. [Crossref] [PubMed]
- Schouten N, Simmermacher RK, van Dalen T, et al. Is there an end of the ‘‘learning curve’’ of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 2013;27:789-94. [Crossref] [PubMed]
- Lowham AS, Filipi CJ, Fitzgibbons RJ, et al. Mechanisms of hernia recurrence after preperitoneal mesh repair: traditional and laparoscopic. Ann Surg 1997;225:422e31.
- Felix E, Scott S, Crafton B, et al. Causes of recurrence after laparoscopic hernioplasty. A multicenter study. Surg Endosc 1998;12:226-31. [Crossref] [PubMed]
- Burcharth J, Pommergaard HC, Bisgaard T, et al. Patient-related risk factors for recurrence after inguinal hernia repair: A systematic review and meta-analysis of observational studies. Surg Innov 2015;22:303-17. [Crossref] [PubMed]
- Weyhe D, Klinge U. Meshes. Chapter 10. HerniaSurge Guidelines Part 1. Available online: www.herniasurge.com
- Fortelny RH, Sanders DL, Montgomery A. Mesh fixation. Chapter 11. HerniaSurge Guidelines Part 1. Available online: www.herniasurge.com
- Niebuhr H, Pawlak M, Śmietański M. Diagnostic Testing Modalities. Chapter 3. HerniaSurge Guidelines Part 1. Available online: www.herniasurge.com
- van den Heuvel BJ, Wijsmuller AR, Fitzgibbons RJ. Indications - Treatment Options for Symptomatic and Asymptomatic Patients. Chapter 5. HerniaSurge Guidelines Part 1. Available online: www.herniasurge.com
- Tran H, Weyhe D, Berrevoet F. Recurrent Inguinal Hernias. Chapter 20. HerniaSurge Guidelines Part 2. Available online: www.herniasurge.com
- Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia Surg Endosc 2011;25:2773-843. [International Endohernia Society (IEHS)]. [Crossref] [PubMed]
- Bittner R, Montgomery MA, Arregui ME, et al. Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 2015;29:289-321. [Crossref] [PubMed]
- Sevonius D, Gunnarsson U, Nordin P, et al. Recurrent groin hernia surgery. Br J Surg 2011;98:1489. [Crossref] [PubMed]
- Dedemadi G, Sgourakis G, Radtke A, et al. Laparoscopic versus open mesh repair for recurrent inguinal hernia: a meta-analysis of outcomes. Am J Surg 2010;200:291. [Crossref] [PubMed]
- Karthikesalingam A, Markar SR, Holt PJ, et al. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg 2010;97:4. [Crossref] [PubMed]
Cite this article as: Sharma A, Sarwal A. Surgical repair in recurrent inguinal hernia. Ann Laparosc Endosc Surg 2017;2:97.