Total extraperitoneal approach in inguinal hernia repair: an update
Introduction
The pathophysiology of the posterior endoscopic approach is based on the use of a large prosthesis to overlap the myopectineal orifice of Fruchaud and is well reproduced in the total extraperitoneal (TEP) repair. In TEP, by avoiding to enter the peritoneum, we have a reduced risk of bowel and vascular injury, no postoperative adhesions and the advantages of lower recurrence and complication rates with an overall better outcome (1,2).
Preoperative assessment and surgical technique
There some relative contraindications strongly dependently on the surgeon’s experience and, as in all surgical patients, some absolute contraindications (Acute abdomen with strangulated and infected bowel, Respiratory distress). In patients with irreducible, sliding or inguinoscrotal hernia, previous prostatectomy or pelvic surgery the surgical experience in endo-laparoscopic hernia repair is very important for the success; similarly for example a repair after an open appendectomy it will requires a special attention during the dissection of the lateral space of Bogros.
As all inguinal hernia, a simple physical examination is important to assess the patient including the fitness for general anesthesia. Only in selected case like large inguinoscrotal or multiple recurrence, a dynamic US or a CT scan may be indicated.
Risk for conversion to either TAPP or open, recurrence and complications should be adequately discussed and commented to the patient (3).
As stated from the several Guidelines, in TEP antibiotic are not necessary, we recommend only in case of older patients or selected case like corticosteroid use, immunosuppressive conditions, BPH, obesity, diabetes (4-6).
A urinary catheter is recommended only in complex cases (partially reducible, large defect) or if the surgery last more than 1.5 h.
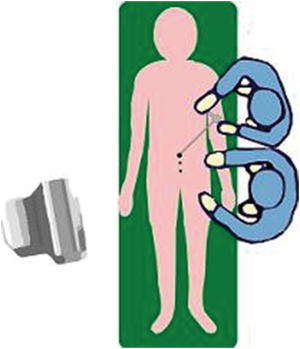
The TEP procedure is standardly performed under general anesthesia, patient is positioned in supine position.
The surgeon and the camera holding assistant stand on the opposite side the hernia. (Figure 1) The high-definition 2D or 3D camera system is positioned at the feet of the patient.
The most common techniques to access and create the preperitoneal space are the balloon dissector or the blunt technique. After incising the anterior rectus sheath, the rectus mm is retracted and the retrorectal space exposed. Using the trocar with an optical balloon dissector, the space is created by inflating the balloon under vision (Figure 2) an be performed initially with a gauze or a finger then using the telescopy along the midline and towards the pubis symphysis in order to allow the position of the two working lower 5 mm trocars. Once all the ports are inserted, using two atraumatic graspers, the dissection is conducted along the midline, below the rectus muscle and towards the pubis arch. The limit of the dissection is 2 cm beyond the symphysis pubis. Subsequently, the lateral dissection is performed towards the anterior superior iliac spine (ASIS) in the so-called lateral space of Bogros. Attention should be made to avoid to dissect beyond the lumbar fascia in the so-called “lateral triangle of pain”. This will prevent injury of the lateral-cutaneous and genitofemoral nerves
Once the preperitoneal dissection is completed, the hernia defects are identified and the next step will be the sac reduction and repair of the hernia. An adequate dissection both lateral and medial is necessary for the placement of the 10 cm × 15 cm prosthesis and to work safely in case of inadvertent tear of the peritoneum.
The reduction of direct, femoral and obturator hernia are simple and requires attention to avoid injury of the surrounding vasculat structures. For the indirect or lateral hernia this will requires to separate the spermatic structures from the hernia sac using either the preferred medial to lateral approach. In case of long, large or difficult thick sac, it is advisable to transect the hernia sac over a simple ligation of using a pre-made loop. If a lipoma of the cord is present it will required to be fully reduced.
It is important to close all the inadvertent peritoneal holes/tears with absorbable suture or loops.
The final step is the hernia repair and it is achieved by covering all the myopectineal orifice of Fruchaud with a synthetic, large pore prosthesis of at least 10 cm × 15 cm. The insertion of the rolled mesh is done through the 10 mm trocar. A “no-touch technique” is mandatory to avoid mesh infection. The mesh is opened and inserted into the preperitoneal cavity avoiding any contact with the skin. The mesh is then placed horizontally and unrolled over the myopectineal orifice making sure to cover all the hernia sites (Figure 3). One third of the mesh should be below the symphysis pubis, the upper margin reaching the lower trocar medially and laterally lining over the psoas muscle. In case of bilateral hernias, the two meshes should overlap 1–2 cm over the midline. The peritoneum should be at least 1–2 cm away from the inferior edge of the mesh to prevent a recurrence.
The fixation of the mesh is required only in large direct or indirect hernia or in case of bilateral repair. Four to five staplers over the Cooper’s ligament, medial and lateral to the inferior epigastric vessels are sufficient for good fixation. We should avoid any stapler below the iliopubic tract because there are nerve path abnormalities in 15–20% of the case. This will help to prevent any nerve injuries and consequent post-operative chronic pain.
At the end of the procedure, the anterior rectus sheath is closed with non-absorbable suture and the skin using glue or subdermal suture.
Patients can be discharged on the same day after voiding freely with standard NSAID analgesia.
Single or reduced port technique
As in many other procedures, also in endolaparoscopic hernia repair, we have utilized a reduced or single access approach (7,8). For needlescopic surgery, 2–3 mm trocars and grasper are utilized to perform the procedure, challenges are in large defect or thickened peritoneal sac. Clinical studies showed comparable results with standard technique but nevertheless, the needlescopic technique has never been successful with worldwide acceptance (7,9). Lately, the repair using a single port device (Figure 4) have been popularized and has seen a lot of enthusiasm not only for inguinal hernia repair but for several surgical procedure and commonly appendectomy, cholecystectomy, adrenalectomy, cystectomy, appendectomy, colon surgery, etc. (10-14). One of the advantages claimed for the single or reduced port surgery is the better cosmetic, lesser pain and faster recovery while the increased risk for port-site hernia can be an important side effect, even though this is not claimed for TEP. On the other side the technical challenges are the lack in triangulation, the difficult in achieving a proper retraction (15). In TEP these challenges are relative, since the position on the trocars along the midline partially simulates a lack of triangulation and this help to shorten the learning curve for single port surgery.
Recent comparative studies showed similar data regarding pain scores, operative duration, recurrence and complication rates, making this new approach acceptable and comparable to standard TEP (16,17).
Clinical outcome and complications
Intraoperative complications specific to TEP occur a very low percentage in about 4–6% of the cases and can be due to vascular, visceral, nerve and spermatic cord structures injury (3,18-21). The most common are the injury of the IEV and this can be avoided by inserting all the ports under direct vision and with a careful lateral dissection. Visceral injuries are very rare with few reports in the literature, may be due to excessive traction in reducing a sac with bowel content or by transmitted energy. Nerve injuries can be prevented by avoiding lateral dissection beyond the lumbar fascia and by limiting the numbers of staplers/tacker for fixation.
Postoperative complication like seroma commonly occur in patients with large direct and indirect hernia, the seroma usually appear after 7–10 days and do not require any treatment and will be reabsorbed spontaneously within 4–6 weeks (21-23).
TEP hernia repair has showed in several clinical trials and metanalysis that has reduced postoperative pain, less need for postoperative analgesia, earlier return at work, fewer complications and low recurrence in experienced surgeon when compared to open mesh repair (1,2) and this is also stated in the several Guidelines published (4-6,22,23). The key of a successful TEP repair is in the patient’s selection and a correct surgical technique together with the surgeon’s experience, only these three key factors will allow to achieve a good clinical outcome with low rate of short and long-term complications.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery for the series “Inguinal Hernia Repair”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2017.07.12). The series “Inguinal Hernia Repair” was commissioned by the editorial office without any funding or sponsorship. DL served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Jun 2016 to May 2018. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Memon MA, Cooper NJ, Memon B, et al. Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 2003;90:1479-92. [Crossref] [PubMed]
- Karthikesalingam A, Markar SR, Holt PJ, et al. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br J Surg 2010;97:4-11. [Crossref] [PubMed]
- Lomanto D, Katara AN. Managing intra-operative complications during totally extraperitoneal repair of inguinal hernia. J Minim Access Surg 2006;2:165-70. [Crossref] [PubMed]
- Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009;13:343-403. [Crossref] [PubMed]
- Miserez M, Peeters E, Aufenacker T, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2014;18:151-63. [Crossref] [PubMed]
- Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia Surg Endosc 2011;25:2773-843. [International Endohernia Society (IEHS)]. [Crossref] [PubMed]
- Goo TT, Lawenko M, Cheah WK, et al. Endoscopic total extraperitoneal repair of recurrent inguinal hernia: a 5-year review. Hernia 2010;14:477-80. [Crossref] [PubMed]
- Lau H, Lee F. A prospective comparative study of needlescopic and conventional endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 2002;16:1737-40. [Crossref] [PubMed]
- Goo TT, Goel R, Lawenko M, et al. Laparoscopic transabdominal preperitoneal (TAPP) hernia repair via a single port. Surg Laparosc Endosc Percutan Tech 2010;20:389-90. [Crossref] [PubMed]
- Wada H, Kimura T, Kawabe A, et al. Laparoscopic transabdominal preperitoneal inguinal hernia repair using needlescopic instruments: a 15-year, single-center experience in 317 patients. Surg Endosc 2012;26:1898-902. [Crossref] [PubMed]
- Trastulli S, Cirocchi R, Desiderio J, et al. Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg 2013;100:191-208. [Crossref] [PubMed]
- Fung AK, Aly EH. Systematic review of single-incision laparoscopic colonic surgery. Br J Surg 2012;99:1353-64. [Crossref] [PubMed]
- Rehman H, Mathews T, Ahmed I. A review of minimally invasive single-port/incision laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A 2012;22:641-6. [Crossref] [PubMed]
- Goo TT, Agarwal A, Goel R, et al. Single-port access adrenalectomy: our initial experience. J Laparoendosc Adv Surg Tech A 2011;21:815-9. [Crossref] [PubMed]
- Goel R, Lomanto D. Controversies in single-port laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 2012;22:380-2. [Crossref] [PubMed]
- Fuentes MB, Goel R, Lee-Ong AC, et al. Single-port endo-laparoscopic surgery (SPES) for totally extraperitoneal inguinal hernia: a critical appraisal of the chopstick repair. Hernia 2013;17:217-21. [Crossref] [PubMed]
- Wijerathne S, Agarwal N, Ramzi A, et al. Single-port versus conventional laparoscopic total extra-peritoneal inguinal hernia repair: a prospective, randomized, controlled clinical trial. Surg Endosc 2016;30:1356-63. [Crossref] [PubMed]
- Tetik C, Arregui ME, Dulucq JL, et al. Complications and recurrences associated with laparoscopic repair of groin hernias. A multi-institutional retrospective analysis. Surg Endosc 1994;8:1316-22; discussion 1322-3. [Crossref] [PubMed]
- Kraus MA. Nerve injury during laparoscopic inguinal hernia repair. Surg Laparosc Endosc 1993;3:342-5. [PubMed]
- Felix EL, Harbertson N, Vartanian S. Laparoscopic hernioplasty: significant complications. Surg Endosc 1999;13:328-31. [Crossref] [PubMed]
- Miguel PR, Reusch M, daRosa AL, et al. Laparoscopic hernia repair--complications. JSLS 1998;2:35-40. [PubMed]
- Cavazzola LT, Rosen MJ. Laparoscopic versus open inguinal hernia repair. Surg Clin North Am 2013;93:1269-79. [Crossref] [PubMed]
- Bittner R, Montgomery MA, Arregui E, et al. Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 2015;29:289-321. [Crossref] [PubMed]
Cite this article as: Lomanto D, Sta. Clara EL. Total extraperitoneal approach in inguinal hernia repair: an update. Ann Laparosc Endosc Surg 2017;2:119.