
Evolution of minimally invasive pancreatic surgery in Thailand
The first minimally invasive pancreatic surgery was performed by Gagner et al. in 1993 when laparoscopic distal pancreatectomy was successfully done (1). In 1994, Gagner and Pomp performed the first laparoscopic pancreaticoduodenectomy (2). However, minimally invasive pancreatic surgery was very slowly adopted in surgical community because of difficulty to access by laparoscope due to its retroperitoneal location. Moreover, its unproven benefit led to a high degree of scepticism regarding a major change in practice. Nevertheless, a group of surgeons continued to develop this minimally invasive pancreatic surgery. After Da Vinci robot was introduced, Melvin et al. reported the first robotic pancreatic surgery in 2003 (3). The cost of Da Vinci robotic system is a main obstacle to the widespread use of robotic surgery. On the contrary, laparoscopic pancreatic surgery has been accepted as an alternative treatment in many centers (4,5). When single incision laparoscopic surgery was successfully performed in many organs (6-10), this technique was also successfully attempted in pancreatic surgery (11,12). However, single incision laparoscopic is not popular among surgeons because of the highly technical demanding skill and questionable benefit to the patient (13,14).
To date, many studies have shown that the results of laparoscopic distal pancreatectomy in benign and low grade malignant pancreatic disease are comparable to open distal pancreatectomy with possible better perioperative outcome. Therefore, they are accepted as an alternative to standard surgery in many centers (4,5). Currently, the surgical technique of laparoscopic distal pancreatectomy is settled.
Laparoscopic pancreaticoduodenectomy also has favorable results in comparison to open pancreaticoduodenectomy including oncologic outcome (15,16) and better survival in some reports (17). However, laparoscopic pancreaticoduodenectomy is not widely accepted as an alternative treatment, only few centers adopted this surgery for treatment of periampullary lesions due to the complexity of the operation and the questionable benefit to the patients.
Minimally invasive pancreatic surgery was first done in Thailand at King Chulalongkorn Memorial Hospital when Professor Patpong Navicharern successfully performed laparoscopic-assisted pancreaticoduodenectomy in 2008. One year later, he also successfully performed laparoscopic distal pancreatectomy. The first pure laparoscopic pancreaticoduodenectomy was successfully done by Dr. Araya Khaimook at Hatyai Hospital in 2009. Laparoscopic distal pancreatectomy has been developed as an alternative treatment in most of university hospitals and some tertiary hospitals in Thailand. However, this surgical technique has not gained popularity due to its high cost. In the meantime, laparoscopic pancreaticoduodenectomy was developed in only some centers because complexity of the operation and very steep learning curve. In 2009 when Da Vinci robot was available in Thailand, the first robotic pancreaticoduodenectomy was done at Siriraj Hospital by Professor Anusak Yiengpreuksawan, a visiting surgeon from The Valley Hospital in New Jersey, United States. In contrast to laparoscopic pancreatic surgery, robotic pancreatic surgery has not gained surgical ground due to its very high cost. During 2010–2014 laparoscopic pancreatic surgery slowly gained popularity among university hospitals and super-tertiary hospitals. The new technique of laparoscopic pancreaticoduodenectomy was pioneered in 2014 when the author introduced laparoscopic left posterior approach superior mesenteric artery (SMA) first pancreaticoduodenectomy, which was developed from original technique proposed by Kurosaki et al. (18) for open SMA first approach pancreaticoduodenectomy. Since then, laparoscopic pancreaticoduodenectomy with various techniques has been adopted in many centers and become an option for selected patients with periampullary carcinoma.
So far, minimally invasive pancreatic surgery has been done in at least eight medical centers in Thailand. Approximately 180 Thai patients received these minimally invasive pancreatic surgeries including 50 cases of laparoscopic distal pancreatectomy, 60 cases of laparoscopic pancreaticoduodenectomy, 70 cases of laparoscopic assisted pancreaticoduodenectomy, a few cases of laparoscopic enucleation and robotic pancreatic surgery (unpublished data).
Rajavithi Hospital, the largest hospital in Ministry of Public Health, is one of the most active center in laparoscopic pancreatic surgery. As mentioned above, the laparoscopic left posterior approach SMA first pancreaticoduodenectomy was pioneered by the author at this hospital. In 2010, the first laparoscopic pancreatic surgery initiated at Rajavithi Hospital was laparoscopic distal pancreatectomy. Then, in 2013, the first laparoscopic assisted pancreaticoduodenectomy was done. Finally, total laparoscopic pancreaticoduodenectomy was successfully done by left posterior SMA first approach in 2014. So far, there are 60 cases of laparoscopic pancreatic surgery, including 35 cases of laparoscopic pancreaticoduodenectomy by our technique, 24 cases of laparoscopic distal pancreatectomy, and one case of laparoscopic enucleation. However, we do not have experience in laparoscopic middle pancreatectomy (unpublished data).
Methods: surgical technique
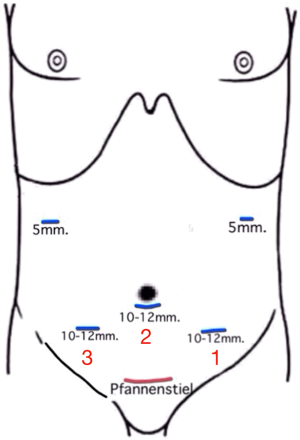
The technique of laparoscopic left posterior approach SMA first pancreaticoduodenectomy, which is routinely used at Rajavithi Hospital, can be described as ‘3 fields of dissection and 2 fields of reconstruction’ using 5 ports (Figure 1). The dissection fields are SMA, central and right subhepatic field (Figure 1). The reconstruction is done in SMA and right subhepatic field. The surgery is commenced at SMA field by dissection into retroperitoneal space to expose aorta and inferior vena cava (IVC) and to identify SMA root. Then SMA is dissected from left posterior side to free it from uncinate process and surrounding tissue, then the inferior pancreaticoduodenectomy artery (IPDA) is identified and divided. At central field, the lesser sac is widely opened to expose anterior surface of pancreas with mobilization of hepatic flexure of colon, then gastroepiploic vessels and Henle’s trunk are identified and divided. Final stage of dissection is done in right subhepatic field by Kocherization of duodenum, transection of antrum, transection of pancreas and transection of biliary tract to complete the resection. After specimen is removed through Pfannenstiel incision, pancreaticojejunostomy is first done follow by hepaticojejunostomy in right subhepatic field. Then the operation is completed with gastrojejunostomy in central field.
Results
The results of 35 cases of laparoscopic left posterior approach SMA first pancreaticoduodenectomy at Rajavithi Hospital are as follows. There were eleven females and 24 males, the average age was 59.6 years. Average body mass index was 22.33±3.05 kg/m2. The most common diagnosis was ampullary carcinoma (Table 1). Major morbidity occurred in 6 cases (17.1%) (Table 2), mortality 2 cases (5.7%). One mortality occurred from cardiogenic cause and another case had leakage of biliary anastomosis which was complicated by fatal post pancreatectomy hemorrhage. Average operative time was 599.52±119.85 minutes. Average blood loss (including conversion cases) was 1,512±1,214 mL, while blood loss in successful laparoscopic left posterior approach SMA first pancreaticoduodenectomy cases was 776±399 mL. The explanation for the difference in blood loss is almost all conversion cases (six of seven cases) had injury of branch of portal vein. The outcome was comparable to open technique in our center (unpublished data).
Table 1
| Diagnosis | Number | Conversion | % |
|---|---|---|---|
| Ampullary carcinoma | 18 | 3* | 16.7 |
| Cystic tumor (IPMN, SPN, etc.) | 5 | 0 | 0 |
| Distal cholangiocarcinoma | 4 | 0 | 0 |
| Pancreatic head CA | 3 | 0 | 0 |
| Duodenal carcinoma | 3 | 2 | 66.7 |
| Chronic inflammation | 2 | 2 | 100 |
| Total | 35 | 7 | 20 |
*, abbreviation; CA, carcinoma; IPMN, intraductal papillary mucinous neoplasm; SPN, solid pseudopapillary neoplasm.
Table 2
| Morbidity | Number | % |
|---|---|---|
| Pancreatic fistula | 2 | 5.7 |
| Biliary leakage | 2 | 5.7 |
| Post pancreatectomy hemorrhage | 1 | 2.8 |
| Pulmonary embolism | 1 | 2.8 |
| Total | 6 | 17.1 |
In conclusion, minimally invasive pancreatic surgery has been developed for more than two decades but it has been slowly accepted. Finally, laparoscopic distal pancreatectomy is accepted as an option for benign and low grade malignant tumor. However, laparoscopic pancreaticoduodenectomy is still in the developing process and is an option in only few centers. In Thailand, minimally invasive pancreatic surgery is in the beginning phase, only few hundred cases are treated with this technique. Nevertheless, Rajavithi Hospital is one of most active hospital in this minimally invasive pancreatic surgery, and the author has successfully developed technique of laparoscopic left posterior approach SMA first pancreaticoduodenectomy with comparable results to open technique. Laparoscopic distal pancreatectomy should be a standard treatment for all pancreatic body and tail lesions in the near future. However, for laparoscopic pancreaticoduodenectomy being accepted as a standard treatment, more studies will be needed to prove the benefit to the patients.
Acknowledgments
The author would like to thank Professor Patpong Navicharern, Dr. Araya Khaimook, Dr. Vor Luvira, Dr. Tharatip Srisuk, Dr. Prawat Kositamongkol and Assistant Professor Chatchai Mingmalairak for providing information of minimally invasive pancreatic surgery.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Chung Yip Chan, Ser Yee Lee and Adrian Kah Heng Chiow) for the series “Advanced Laparoscopic HPB Surgery in South East Asia” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.05.08). The series “Advanced Laparoscopic HPB Surgery in South East Asia” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gagner M, Pomp A, Herrera MF. Early experience with laparoscopic resections of islet cell tumors. Surgery 1996;120:1051-4. [Crossref] [PubMed]
- Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreaticoduodenectomy. Surg Endosc 1994;8:408-10. [Crossref] [PubMed]
- Melvin WS, Needleman BJ, Krause KR, et al. Robotic resection of pancreatic neuroendocrine tumor. J Laparoendosc Adv Surg Tech A 2003;13:33-6. [Crossref] [PubMed]
- Kim SC, Park KT, Hwang JW, et al. Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surg Endosc 2008;22:2261-8. [Crossref] [PubMed]
- Nakamura M, Wakabayashi G, Miyasaka Y, et al. Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepatobiliary Pancreat Sci 2015;22:731-6. [Crossref] [PubMed]
- Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A 1999;9:361-4. [Crossref] [PubMed]
- Remzi FH, Kirat HT, Kaouk JH, et al. Single-port laparoscopy in colorectal surgery. Colorectal Dis 2008;10:823-6. [Crossref] [PubMed]
- Reavis KM, Hinojosa MW, Smith BR, et al. Single-laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg 2008;18:1492-4. [Crossref] [PubMed]
- Ponsky LE, Cherullo EE, Sawyer M, et al. Single access site laparoscopic radical nephrectomy: Initial clinical experience. J Endourol 2008;22:663-6. [Crossref] [PubMed]
- Misawa T, Sakamoto T, Ito R, et al. Single-incision laparo-scopic splenectomy using the “tug-exposure technique” in adults: Results of ten initial cases. Surg Endosc 2011;25:3222-7. [Crossref] [PubMed]
- Barbaros U, Sümer A, Demirel T, et al. Single incision laparoscopic pancreas resection for pancreatic metastasis of renal cell carcinoma. JSLS 2010;14:566-70. [Crossref] [PubMed]
- Kuroki T, Adachi T, Okamoto T, et al. Single-incision laparoscopic distal pancreatectomy. Hepatogastroenterology 2011;58:1022-4. [PubMed]
- Wong JS, Cheung YS, Fong KW, et al. Comparison of Postoperative Pain Between Single-incision Laparoscopic Cholecystectomy and Conventional Laparoscopic Cholecystectomy: Prospective Case-control Study. Surg Laparosc Endosc Percutan Tech 2012;22:25-8. [Crossref] [PubMed]
- Ma J, Cassera MA, Spaun GO, et al. Randomized Controlled Trial Comparing Single-Port Laparoscopic Cholecystectomy and Four-Port Laparoscopic Cholecystectomy. Ann Surg 2011;254:22-7. [Crossref] [PubMed]
- Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 2012;215:810-9. [Crossref] [PubMed]
- Boggi U, Amorese G, Vistoli F, et al. Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc 2015;29:9-23. [Crossref] [PubMed]
- Croome KP, Farnell MB, Que FG, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg 2014;260:633-40. [Crossref] [PubMed]
- Kurosaki I, Minagawa M, Takano K, et al. Left posterior approach to the superior mesenteric vascular pedicle in pancreaticoduodenectomy for cancer of pancreatic head. JOP 2011;12:220-9. [PubMed]
Cite this article as: Treepongkaruna SA. Evolution of minimally invasive pancreatic surgery in Thailand. Ann Laparosc Endosc Surg 2018;3:52.


