Combined totally extraperitoneal preperitoneal repair and laparoscopic appendectomy for treatment of an asymptomatic, incarcerated Amyand’s hernia in an adult
Introduction
Herniation of the vermiform appendix into the inguinal canal was first described in 1736 by Claudius Amyand, and now bears his eponym (Amyand’s hernia). Modern studies assessing its prevalence have reported it in 0.14–0.6% of inguinal hernias in adults (1-5), and in 0.4–1.0% of pediatric hernias (4,6-9). The majority of pediatric patients with Amyand’s hernias presented with asymptomatic inguinal hernias in all of the largest case series available (1,7). In adults, however, the two largest case series both reported that 100% of their diagnoses were made during emergency surgical intervention for presumed strangulated or incarcerated hernias (3,5), and only a small number of asymptomatic cases are reported in available literature (10). None of these asymptomatic appendices were incarcerated. Preoperative diagnosis with imaging is exceedingly rare, as incarcerated and strangulated hernias tend to be diagnosed clinically (11). We report an unusually asymptomatic presentation of this rare hernia, describe our minimally invasive approach to its reduction, and discuss salient decisions made during the procedure. This is the sole known report of a combination of totally extraperitoneal preperitoneal (TEP) repair with intraperitoneal laparoscopic appendectomy for treatment of an incarcerated Amyand’s hernia, as well as the only known report of an asymptomatic incarcerated Amyand’s hernia.
Case presentation
The patient was a 71-year-old man who presented to outpatient clinic with one month of a generally painless bulge in his right groin. He had a history of right sided inguinal hernia repair 7 years prior, which was performed without mesh to accommodate the patient’s preference against placement of a permanent prosthetic. On presentation, his vitals were stable and he was noted to have a 3 cm by 3 cm, non-reducible mass in the right groin that was only mildly tender to palpation and consistent with a recurrent right inguinal hernia. He had no other complaints. He was scheduled for elective hernia repair three weeks later via a TEP approach using a resorbable mesh (Ventralight), again due to patient preference.
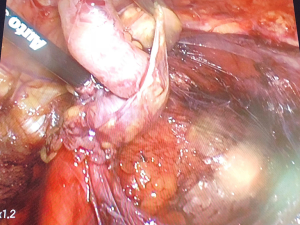
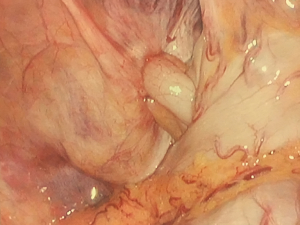
On the day of his outpatient surgery, after infusion of cefazolin, the preperitoneal space was accessed via a 10-mm incision to the left of the umbilicus, and the laparoscope was inserted into this port. Two 5-mm ports were placed inferiorly in the midline for instrumentation. The space was dissected until the anatomic landmarks were clear and the spermatic cord contents were isolated, at which point it became apparent that a hernia sac was present adjacent to the cord, through which the patient’s appendix emerged (Figure 1). The appendix lacked inflammation (Figure 2) but was large and incarcerated. Reduction of the appendix into the abdomen could not be performed nor could the base of the appendix be visualized from the preperitoneal space. The decision was made to place the absorbable mesh around the cord, deflate the preperitoneal space, and convert to an intraperitoneal approach for reduction without making new incisions.
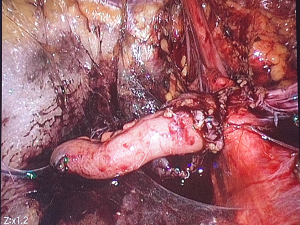
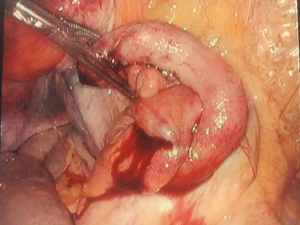
On entry, the patient’s otherwise healthy vermiform appendix was observed to be incarcerated in the defect (Figure 3). We then proceeded to manually dilate the peritoneal defect with dissecting forceps while applying traction to the base of the appendix and were able to achieve complete reduction. The defect was closed with an endoloop and the appendix was subsequently stapled in standard fashion due to ischemic changes that were noted after reduction (Figure 4). There was no perforation of the appendix and no prophylactic antibiotics were prescribed postoperatively. Histologic evaluation of the appendix revealed serosal adhesions without other abnormalities. The patient was discharged the same day and has had no complications to date on follow up.
Discussion
Due to the rarity of the defect, information regarding the presentation and management of Amyand’s hernia in an adult comes entirely from case reports and series. One such series reports 18 cases in a 15-year time period at a single institution, all of which underwent open emergency inguinal hernia repair for clinical diagnoses of strangulated hernias and all of which were diagnosed intraoperatively (5). Emergent surgical intervention in the treatment of Amyand’s hernia is also described in many other available case reports (3,12), although appendicitis within Amyand’s hernia only makes up approximately 0.1% of cases of appendicitis (3-5,13,14). Our current report is unique in that it demonstrates the finding of an asymptomatic, incarcerated appendix within the hernia sac. Based on intraoperative observations, we expect that this patient would have developed strangulation or appendicitis in the near future. It is conceivable that the insufflation in the preperitoneal space worsened incarceration of an otherwise mobile appendix, though the defect was small relative to the size of the appendix and strongly suggested chronic incarceration.
In this case, we elected to continue our minimally invasive approach without converting to an open approach or introducing new ports. The majority of available case reports and series discuss open hernia repair necessitated by the urgent presentation of these hernias, with or without appendectomy (5). Appendectomy has been performed via the inguinal incision, through an open abdominal incision, or through laparoscopy. From a TEP repair, no case reports have clearly identified appendectomy performed in the preperitoneal space or via conversion to laparoscopy. There have been reports of preperitoneal management without appendectomy for reducible hernias (10) as well as laparoscopic management of the appendix with delayed repair of the hernia defect for treatment of acute appendicitis (15,16). Our case is the sole known report of a non-reducible appendix identified during TEP with successful repair of the hernia and successful intraabdominal reduction and excision of the appendix. We feel that continued laparoscopic management is a safe option in a case of Amyand’s hernia that is diagnosed during routine laparoscopic preperitoneal inguinal hernia repair, even when the appendix is incarcerated or appendectomy is necessary. The same port sites used to access the preperitoneal space can be used for abdominal access and appendectomy without increased morbidity to the patient.
In addition to minimizing recovery time and patient discomfort, our approach also minimized the risk of infection of the mesh. It is suggested by several authors that a Bassini or other mesh-free repair be undertaken in any case that requires appendectomy due to the risk of abdominal contamination and infection of the mesh (5,17). In our method, the defect in the peritoneum was closed and the preperitoneal space was isolated from the abdominal cavity prior to appendectomy. In addition, there was no appendiceal perforation during reduction. The use of mesh has not been shown to increase risks of infection or other complications in considerably more extensive colorectal procedures (18). We therefore felt that appendectomy in this case was not a contraindication to a mesh repair. We would still favor a mesh free repair in the case of appendiceal perforation within the preperitoneal space, as has been reported (4). Another consideration to reduce mesh infection risk includes prophylactic postoperative antibiotics.
It is not always necessary to remove the appendix in a case of Amyand’s hernia. One review recommended a four-tiered classification scheme [1–4] based on the appearance of the appendix, and suggested that type 1 hernias without visible inflammation of the appendix can be managed without appendectomy, preferring appendectomy only in younger patients (19). There have been no studies to validate this classification scheme, but other authors discuss similar management under the paradigm that appendectomy slightly increases the risk of infection (4,11,17). An exception is the report of five patients who underwent open mesh hernia repair and appendectomy without an inflamed appendix and did well postoperatively (20). We agree that a healthy appendix need not be excised if it is easily reduced into the abdomen. In this case, we elected to perform appendectomy due to the ischemic appearance of the appendiceal tip after reduction. The threshold to remove the appendix in order to avoid future appendectomy should be low if the perceived risk of appendectomy is also low.
In conclusion, Amyand’s hernias in adults tend to be diagnosed intraoperatively after presenting with symptoms of incarcerated or strangulated hernia. Our report demonstrates that the diagnosis of an incarcerated Amyand’s hernia is not excluded by an asymptomatic clinical presentation. When it is discovered during TEP repair of the hernia, mesh repair can be performed in the preperitoneal space and conversion to intra-abdominal laparoscopy can preserve a minimally invasive approach. This method isolates the mesh from the abdomen and may reduce the risk of infection of the mesh if appendectomy is performed.
Acknowledgments
We would like to acknowledge Katherine Dailey, RN, and George Rowand, RN, for their assistance during the surgical procedure. We would like to thank our patient for giving his consent to report this case.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.11.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- D'Alia C, Lo Schiavo MG, Tonante A, et al. Amyand's hernia: case report and review of the literature. Hernia 2003;7:89-91. [Crossref] [PubMed]
- Gurer A, Ozdogan M, Ozlem N, et al. Uncommon content in groin hernia sac. Hernia 2006;10:152-5. [Crossref] [PubMed]
- Inan I, Myers PO, Hagen ME, et al. Amyand's hernia: 10 years' experience. Surgeon 2009;7:198-202. [Crossref] [PubMed]
- Michalinos A, Moris D, Vernadakis S. Amyand's hernia: a review. Am J Surg 2014;207:989-95. [Crossref] [PubMed]
- Sharma H, Gupta A, Shekhawat NS, et al. Amyand's hernia: a report of 18 consecutive patients over a 15-year period. Hernia 2007;11:31-5. [Crossref] [PubMed]
- Cankorkmaz L, Ozer H, Guney C, et al. Amyand's hernia in the children: a single center experience. Surgery 2010;147:140-3. [Crossref] [PubMed]
- Cigsar EB, Karadag CA, Dokucu AI. Amyand's hernia: 11years of experience. J Pediatr Surg 2016;51:1327-9. [Crossref] [PubMed]
- Kaymakci A, Akillioglu I, Akkoyun I, et al. Amyand's hernia: a series of 30 cases in children. Hernia 2009;13:609-12. [Crossref] [PubMed]
- Okur MH, Karacay S, Uygun I, et al. Amyand's hernias in childhood (a report on 21 patients): a single-centre experience. Pediatr Surg Int 2013;29:571-4. [Crossref] [PubMed]
- Sahu D, Swain S, Wani M, et al. Amyand's hernia: Our experience in the laparoscopic era. J Minim Access Surg 2015;11:151-3. [Crossref] [PubMed]
- Ivanschuk G, Cesmebasi A, Sorenson EP, et al. Amyand's hernia: a review. Med Sci Monit 2014;20:140-6. [Crossref] [PubMed]
- Velimezis G, Vassos N, Kapogiannatos G, et al. Incarcerated recurrent inguinal hernia containing an acute appendicitis (Amyand hernia): an extremely rare surgical situation. Arch Med Sci 2017;13:702-4. [Crossref] [PubMed]
- Meinke AK. Review article: appendicitis in groin hernias. J Gastrointest Surg 2007;11:1368-72. [Crossref] [PubMed]
- Psarras K, Lalountas M, Baltatzis M, et al. Amyand's hernia-a vermiform appendix presenting in an inguinal hernia: a case series. J Med Case Rep 2011;5:463. [Crossref] [PubMed]
- Al-Ramli W, Khodear Y, Aremu M, et al. A complicated case of amyand's hernia involving a perforated appendix and its management using minimally invasive laparoscopic surgery: A case report. Int J Surg Case Rep 2016;29:215-8. [Crossref] [PubMed]
- Vermillion J, Abernathy S, Snyder S. Laparoscopic reduction of Amyand's hernia. Hernia 1999;3:159-60. [Crossref]
- Shekhani HN, Rohatgi S, Hanna T, et al. Amyand's Hernia: A Case Report. J Radiol Case Rep 2016;10:7-11. [Crossref] [PubMed]
- Benlice C, Gorgun E, Aytac E, et al. Mesh herniorrhaphy with simultaneous colorectal surgery: a case-matched study from the American College of Surgeons National Surgical Quality Improvement Program. Am J Surg 2015;210:766-71. [Crossref] [PubMed]
- Losanoff JE, Basson MD. Amyand hernia: a classification to improve management. Hernia 2008;12:325-6. [Crossref] [PubMed]
- Kose E, Sisik A, Hasbahceci M. Mesh Inguinal Hernia Repair and Appendectomy in the Treatment of Amyand's Hernia with Non-Inflamed Appendices. Surg Res Pract 2017;2017:7696385 [Crossref] [PubMed]
Cite this article as: Johnson SH, Krumeich LN, Mydlowska AK, Morris JB, Dumon KR. Combined totally extraperitoneal preperitoneal repair and laparoscopic appendectomy for treatment of an asymptomatic, incarcerated Amyand’s hernia in an adult. Ann Laparosc Endosc Surg 2018;3:91.