Minimally invasive surgery in vesicoureteric reflux
Introduction
Vesicoureteric reflux (VUR) is a common cause for recurrent urinary tract infection (UTI) in children. There is risk of renal scarring and renal function impairment in patients with recurrent UTI and underlying VUR. The management options and theory has been changing over the last 30 to 40 years since the introduction of endoscopic treatment, laparoscopic surgery and robot-assisted laparoscopic ureteral reimplantation (RALUR). Because of the new advances, there are controversies in selecting the best treatment option. Up till now, there is a debating topic between pediatric urologists on the best treatment option for this group of patients.
Natural history of VUR
VUR is a common condition in children. The estimated incidence of UTI among the age group of 2 to 24 months is around 5% (1). VUR is present in around 30–40% of this group of patients. The overall rates of renal scarring after an episode of acute pyelonephritis with VUR is around 37–41.6% (2). Its severity is graded according to International Reflux Study Committee from grade 1 to 5 (3). In treating VUR, our primary goal is to prevent UTI and hence renal scarring. Yet, not all patients with VUR would have UTI necessarily and we know there is spontaneous resolution of VUR in certain proportion of the patients. Researchers tried to formulate a model to predict the group of patients who will have high chance of spontaneous resolution and hence avoid surgical management. Younger age and lower VUR grading are the favourable factors for spontaneous resolution where presence of bladder bowel dysfunction (BBD) and renal scarring are unfavourable factors. The spontaneous resolution rate for grade 1 VUR at 5 years of age is around 92% and is only 16% for grade IV VUR at the same age (4).
Management
General principles and goal of management
Most patients present with an episode of UTI, but some do present with antenatal hydronephrosis or sibling screening. The aim of treatment is to prevent UTI and hence renal cortical abnormalities (5). There are published guidelines on treatment but no consensus on selection of surgical treatment (5,6). The suggestions concern mainly management of primary VUR. Treatment of secondary VUR with underlying bladder or urethral anomalies involves treatment of the underlying problems. So, presence of BBD is an important factor that clinician should ask or look for before decision on treatment options. Presence of BBD is associated with higher risk of UTI, smaller rate of spontaneous resolution, lower success rate from endoscopic treatment and higher rate of UTI after surgical treatment (5). Constipation and bladder dysfunction should be treated. Prompt treatment of UTI can also help decrease the risk of renal scarring.
There are mainly 3 approaches on VUR treatment, i.e., continuous antibiotics prophylaxis (CAP), endoscopic treatment and ureteric reimplantation (open vs. minimally invasive).
CAP
CAP is an important treatment to prevent UTI in VUR. It is shown to be equally effective in preventing recurrence of UTI (19% and 23% in CAP and endoscopic treatment) as compared with endoscopic treatment and significantly better than active surveillance group without antibiotics prophylaxis (57%) in Swedish Reflux trial (7). The protective effect is also concurred by another randomized controlled trial, RIVUR trial (8), which showed antimicrobial prophylaxis with trimethoprim-sulfamethoxazole reduced the incidence of recurrent UTI by approximately 50% among children with VUR. There is also a strong evidence that prompt treatment of UTI can help decrease the incidence of new renal scarring.
For patients who develop breakthrough UTI while on antibiotics prophylaxis, it is generally agreed that surgical intervention should be considered.
Endoscopic treatment
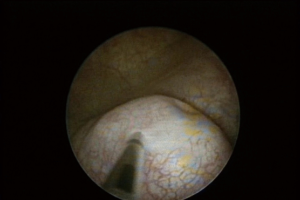
Open ureteral reimplantation has been the only surgical treatment option until 1980s. O’Donnell and Puri published a novel technique of endoscopic subureteral injection of bulking agent Teflon in 1984 (9). It aimed to establish a coapted ureteric channel (Figure 1). Complete absence of VUR was noted in 14 out of 18 ureters after the procedure. Teflon was later abandoned because of its possibility of migration to other parts of the body (10). Endoscopic injection of a relatively biological inert material Dextranomer/hyaluronic acid (Deflux) was introduced in 1995 (11). Its success rate was reported up to 86.5% after 1 injection (12). Most of the patients who had this procedure can be discharged on the same day. With the promising result and noninvasiveness of the procedure, there was a sudden surge in using endoscopic injection as the primary treatment in a way to stop the antibiotic prophylaxis or to avoid the possible morbidities from open ureteral reimplantation. Yet, the success rate was later noted not as great as the initial reports especially in high grade VUR. A systematic review in 2010 showed the complete resolution rate after 1 single injection is 89%, 83%, 71%, 59%, and 62% from grade 1 to grade 5 VUR respectively (13). Success rate decreases with VUR grade increases. Pre-operative VUR grade was the only single important factors in predicting success in this study. Surgeon’s experience, presence of BBD and presence of renal scarring are other factors that may predict success (5,14,15).
Surgeons tried to increase the success rate of high grade VUR by repeated injection. The overall resolution was 69.5% for grade 4–5 patients. Second injection would give a complete resolution in 20.1% of previously failed patient and another 10.4% after third injection (16). Subureteral injection (STING) was the original method of injection. New injection technique “hydrodistension implantation technique” (HIT) was reported to further increase the overall (17) success rate by around 10% (14).
Endoscopic treatment seems to be a good option to be an alternative to ureteral reimplantation. Over the years, long term problems are coming up yet uncommon. Late recurrence of VUR after initial complete resolution was noted. They all presented with recurrence of UTI (18). The rate of UTI recurrence varies in different studies from 0.75% to 27% (19).
There were some scattered case reports on delayed distal ureteric obstruction. They may require either temporary stenting or excision of the vesicoureteric junction and reimplantation (20-22). Histopathology of the excised segment of vesicoureteric junction showed foreign body giant cell reaction and distal intramural fibrosis. There is also a surprising phenomenon of calcified appearance on CT scan or other imaging (18,23). It may mimic unnecessary fear or investigations of possible distal ureteric stone. The density of the material varies in different patients. It was estimated the incidence to be around 2% with around 4 years of lag period after the endoscopic injection to show calcification on ultrasound (23).
When endoscopic treatment is offered to parents, the relative lower success rates and potential long-term problems should be discussed. Both AUA and European Association of Urology (EAU) advised doctors to discuss all the pros and cons of the treatment but did not advise or recommend which surgical options in their guidelines (5,6).
Open reimplantation
Open ureteral reimplantation is the gold standard of treatment of VUR, yet there was no single operative technique as the best technique. Various techniques of open ureteral reimplantation have been reported and can be broadly divided into intravesical and extravesical. VUR can be treated surgically by creating a passive flap valve mechanism that closes the ureters temporarily with elevation of intravesical pressure. Together with construction of a submucosal tunnel with a length to ureteral width ratio of 4–5:1, the intramural part of the ureter is lengthened (19).
Politano and Leadbetter’s (24) intravesical ureteroneocystostomy remains one of the most commonly used technique since its introduction in the 1950s. Intravesical ureteroneocystostomy allows a long submucosal tunnel to be made and maintains the anatomical position of the ureteric orifices for retrograde catheterization. Disadvantages of this popular technique include ureteric kinking, complications of neocystotomy such as obstruction, trans-peritoneal placement and bowel injury.
Refinement in techniques of intravesical ureteric reimplantation techniques had been reported (25-28). Cohen’s intravesical cross-trigonal advancement is another widely used method (27). It allows a long tunnel length and is technically easier to perform. One major disadvantage is the non-anatomical position of ureter that makes retrograde catheterization difficult.
Glenn et al.’s (26) popular surgical approach advances the ureters inferior-medially towards the bladder neck preserving the anatomic alignment of ureters. However, the submucosal tunnel length is rather limited and this technique may not be suitable for dilated ureters.
The major disadvantage of the intravesical technique is that the bladder is split open and postoperative urinary diversion is required. A higher incidence of bladder spasms, higher analgesic requirement and prolonged hospital stay were reported (29) (Table 1).
Table 1
| Operative technique | Brief description of the technique | Pros | Cons |
|---|---|---|---|
| Intra-vesical | |||
| Politano-Leadbetter | Ureter was mobilized in the bladder and re-enter the bladder at a higher position along a submucosal tunnel; ureteric opening will be at its orthotopic site | Maintains anatomical position of ureteric opening | May cause ureteric kinking |
| Cohen | Cross-trigonal advancement of ureteric opening; ureteric opening will be at the other side of the trigone | An easier technique with longer submucosal tunnel | Will have difficulty for retrograde catheterization for later procedure |
| Glenn | Inferior-medial advancement of ureteric opening towards bladder neck | Maintains ureter’s anatomical alignment | Very limited submucosal tunnel length can be created |
| Extra-vesical | |||
| Lich and Gregoir | Submucosal tunnel was created by lateral incision of the detrusor muscle | Avoid problems of bladder spasm, hematuria; long submucosal tunnel with its anatomical alignment can be created | Urinary retention and transient voiding dysfunction were reported for bilateral reimplantation |
The extravesical ureteral reimplantation technique was described by Lich and Gregoir (30,31). Dissection of the ureters is performed to the ureterovesical junction. Lateral incision of detrusor is made along the natural path of the ureter while keeping the mucosa intact and the trigonal attachments to the ureter maintained. A long submucosal tunnel is made by closing the detrusor over the ureter. The extravesical approach does not require bladder opening and has been reported to have reduced incidence of hematuria, bladder spasms, and convalescence (32), and also allows for reimplantation of massively dilated megaureters without tailoring. Nevertheless, the extravesical technique has significant drawbacks. Postoperative urinary retention and transient voiding dysfunction might develop after bilateral reimplantation (33).
Success rates are similar for extra- and intravesical ureteral reimplantation and currently range between 95% and 98% for both open ureteral reimplantation procedures (34). With its high success, open ureteral reimplantation is still regarded as the gold standard for correcting VUR.
Lap reimplantation (extra- and intravesical)
Laparoscopic extravesical ureteral reimplantation was first reported in a pig model by Atala et al. (35) followed by case series in humans (36-38) in 1990s. The patient is placed in light Trendelenburg position. Holding stitches placed through the abdominal wall are used to elevate the bladder. The operation was performed in the way of Lich and Gregoir but in laparoscopic manner. Transverse incision of parietal peritoneum is performed to identify the distal ureter. The detrusor muscle is incised to expose the bladder wall to create a submucosal tunnel by electrocautery. The ureter is placed in the tunnel, and the bladder muscle was closed over the ureter in the tunnel.
Success rates of 88–100% had been reported for minimally invasive ureteric reimplantation (36,39-41). Laparoscopic extravesical Lich-Gregoir ureteric reimplantation has been demonstrated to be safe and effective in treating VUR, with results comparable to open surgery techniques and over sub-ureteral injection techniques (40-42).
Apart from decreased postoperative pain and better cosmesis, this approach allows additional procedures to be performed for other extravesical pathologies such as duplex kidneys. The natural lie of the ureter in the detrusor tunnel and in the abdomen can be visualized, thus ureteral kinking can be avoided. Lower urinary retention rate and shorter hospital stays after laparoscopic bilateral extravesical ureteral reimplantation were reported (43). However, this procedure is technically challenging and operative time is longer, as it requires considerable intracorporeal suturing, meticulous ureteric and detrusor dissection in order to spare the nerve and vas, as well as accomplishment of an adequate submucosal tunnel.
In two long-term series (40,41), VUR disappearance was demonstrated in 85–100% ureters. The incidence of urinary retention was 6.5% in the bilateral group. Complications of ureteral obstruction and urine leakage occurred in 3% patients.
Pneumovesical reimplantation
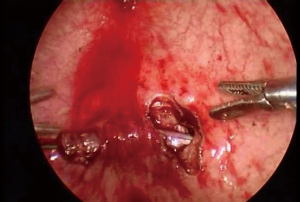
First reported by Yeung et al. (44), the pneumovesical cross-trigonal ureteral reimplantation is now popularized and has better success rates than open cross-trigonal reimplantation. This novel technique combined the advantages of the Cohen’s intravesical cross-trigonal ureteral reimplantation with laparoscopic procedures by creating a pneumovesicum using carbon dioxide (CO2) insufflation of the bladder. Under cystoscopic guidance, a 5-mm camera port was placed over the bladder dome. The bladder was drained and insufflated with CO2. Two more 3- to 5-mm working ports were inserted on the lateral bladder wall on either side. Mobilization of ureter, dissection of a submucosal tunnel and Cohen’s cross-trigonal ureteral reimplantation were performed in an endoscopic intravesical manner (Figure 2).
Chung et al. (45) reported more than 95% success rate was achieved in 9 patients with either VUR or vesicoureteral junction obstruction operated by pneumovesical approach. Cost-effective analysis also favored pneumovesical approach in the study. Intermediate term result from the same center (46) reported outcomes of 42 ureteric reimplantations. Success rate was over 90% and all residual VUR were low-grade and were treated conservatively.
Bi et al. (47) reported their experience of pneumovesical laparoscopic Cohen and excisional ureteral tapering in treating megaureter caused by vesicoureteral junction obstruction. They reported improvement in follow up ultrasound scan and micturating cystourethrogram. One developed ureteral stricture at the neoureterovesical anastomosis requiring reoperation 6 months later.
The pneumovesical Politano-Leadbetter technique (48) had recently been studied and results were compared to that of pneumovesical Cohen technique. Complete VUR resolution occurred in 95% in both groups. There was no difference in the success rate or durations of catheterization or hospital stay.
Robotic reimplantation
Both laparoscopic and pneumovesical ureteral reimplantation are technically challenging procedures with steep learning curve, especially for laparoscopic procedure in a small working space (pediatric patients’ bladder size may be up to 300 mL). There were case series reported mainly in Asia as we have mentioned above. It has not come to popularity worldwide. Minimally invasive ureteric reimplantation accounts for 2.4% of all the pediatric ureteric reimplantation in a study in US (49). RALUR may solve the problem of learning curve.
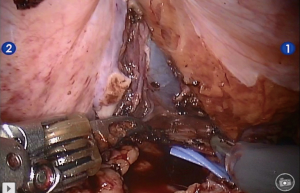
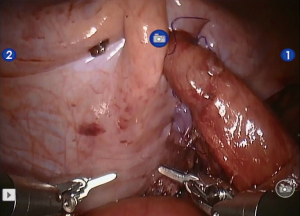
Robot-assisted laparoscopic extravesical ureteral reimplantation (RALUR-EV) was first described by Peters in 2004 (50). This approach has been widely adopted worldwide since. With superior visualization of the robot, mobilization of the ureter is performed close to the adventitia to avoid the neurovascular bundle at the uretero-vesical junction, bladder retraction can also be minimized. Thus, the incidence of postoperative urinary retention can be decreased (Figures 3,4).
Reported RALUR-EV success rates are variable. In some series, success rates are comparable to open reimplantation (51-53). However, the rate was lower (77–92.3%) in other studies (54-57). Various factors may affect success rates, such as tissue handling, electrocautery, tension, extent of ureteral dissection, which very often could not be assessed.
Recent studies also demonstrated a higher complication rate (54,56-60), with an overall major complication up to 13% (60), ureteric obstruction rate up to 7% (57) and ureteral injury rate up to 4%. In the largest cohort of 280 ureters (61), Boysen et al. reported a success rate of 88% and a complication of 10%. Transient urinary retention occurred in 4% following bilateral reimplantation.
The intravesical approach of RALUR has also been introduced (62). Ports are placed in the dome of the bladder and the procedure is performed in a fashion identical to that used for open transtrigonal reimplantation. The robotic instruments facilitate the ureteral mobilization, submucosal tunneling and suturing. In a study on 19 patients, a shorter duration of urinary catheter drainage, fewer bladder spasms, and shorter hospital stays was reported, but the complication rate was higher compared to open (58). Another small series of 3 patients with high-grade bilateral VUR reported 100% reflux resolution (63).
Despite its effectiveness in correcting VUR and other advantages, its use is still limited. It can be attributed by its high costs and availability. Its use is associated with the status of medical insurance and geographical location in US (49).
Circumcision
As the goal of treatment of VUR is prevention of UTI and renal scarring, circumcision is an important treatment modality in VUR management. A meta-analysis in 2005 showed circumcision can reduce the risk of UTI by almost 10-fold (64). Patients with underlying urological anomalies would benefit from circumcision. It should be one of the options that should be included in the management plan of male VUR patients (5,6).
Conclusions
The initial management for VUR should include early recognition of BBD and treatment of constipation. For secondary VUR, the underlying disease must be investigated and tackled accordingly. For mild grade 1–2 primary VUR, expectant management is reasonable, as there is a high chance that spontaneous resolution will occur. Whereas for grade 3 or above VUR, various treatment options including CAP, endoscopic injection and ureteric reimplantation have to be thoroughly discussed with parents. If the patient has high grade VUR and develops breakthrough UTI, surgery have to be considered and the approach is individualized. To date, there is no gold standard or protocol in treating VUR and it still remains a highly debatable topic in the field.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kenneth K. Y. Wong and Patrick Ho Yu Chung) for the series “Paediatric Minimally Invasive Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.11.05). The series “Paediatric Minimally Invasive Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Downs SM. Technical report: Urinary tract infection in febrile infants and young children. The Urinary Tract Subcommittee of the American Academy of Pediatrics Committee on Quality Improvement. Pediatrcs 1999;103:e54 [Crossref] [PubMed]
- Faust WC, Diaz M, Pohl HG. Incidence of post-pyelonephritic renal scarring: a meta-analysis of the dimercapto-succinic acid literature. J Urol 2009;181:290-7; discussion 297-8. [Crossref] [PubMed]
- Lebowitz RL, Olbing H, Parkkulainen KV, et al. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol 1985;15:105-9. [Crossref] [PubMed]
- Routh JC, Bogaert GA, Kaefer M, et al. Vesicoureteral reflux: current trends in diagnosis, screening, and treatment. Eur Urol 2012;61:773-82. [Crossref] [PubMed]
- Peters CA, Skoog SJ, Arant BS Jr, et al. Summary of the AUA Guideline on Management of Primary Vesicoureteral Reflux in Children. J Urol 2010;184:1134-44. [Crossref] [PubMed]
- Tekgül S, Riedmiller H, Hoebeke P, et al. EAU guidelines on vesicoureteral reflux in children. Eur Urol 2012;62:534-42. [Crossref] [PubMed]
- Brandström P, Esbjörner E, Herthelius M, et al. The Swedish reflux trial in children: III. Urinary tract infection pattern. J Urol 2010;184:286-91. [Crossref] [PubMed]
- RIVUR Trial Investigators. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med 2014;370:2367-76. [Crossref] [PubMed]
- O'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed) 1984;289:7-9. [Crossref] [PubMed]
- Steyaert H, Sattonnet C, Bloch C, et al. Migration of PTFE paste particles to the kidney after treatment for vesico-ureteric reflux. BJU Int 2000;85:168-9. [Crossref] [PubMed]
- Stenberg A, Lackgren G. A new bioimplant for the endoscopic treatment of vesicoureteral reflux - experimental and short-term clinical-results. J Urol 1995;154:800-3. [Crossref] [PubMed]
- Puri P, Pirker M, Mohanan N, et al. Subureteral dextranomer/hyaluronic acid injection as first line treatment in the management of high grade vesicoureteral reflux. J Urol 2006;176:1856-9; discussion 1859-60.
- Routh JC, Inman BA, Reinberg Y. Dextranomer/hyaluronic acid for pediatric vesicoureteral reflux: systematic review. Pediatrics 2010;125:1010-9. [Crossref] [PubMed]
- Kirsch AJ, Perez-Brayfield M, Smith EA, et al. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol 2004;171:2413-6. [Crossref] [PubMed]
- Leung L, Chan IHY, Chung PHY, et al. Endoscopic injection for primary vesicoureteric reflux: Predictors of resolution and long term efficacy. J Pediatr Surg 2017;52:2066-9. [Crossref] [PubMed]
- Friedmacher F, Colhoun E, Puri P. Endoscopic Injection of Dextranomer/Hyaluronic Acid as First-Line Treatment in 851 Consecutive Children with High-Grade Vesicoureteral Reflux: Efficacy and Long-Term Results. J Urol 2018;200:650-5. [Crossref] [PubMed]
- Kirsch AJ, Arlen AM. Evaluation of new Deflux administration techniques: intraureteric HIT and Double HIT for the endoscopic correction of vesicoureteral reflux. Expert Rev Med Devices 2014;11:439-46. [Crossref] [PubMed]
- Cerwinka WH, Qian J, Easley KA, et al. Appearance of dextranomer/hyaluronic Acid copolymer implants on computerized tomography after endoscopic treatment of vesicoureteral reflux in children. J Urol 2009;181:1324-8; discussion 1329. [Crossref] [PubMed]
- Marshall S, Guthrie T, Jeffs R, et al. Ureterovesicoplasty: selection of patients, incidence and avoidance of complications. A review of 3,527 cases. J Urol 1977;118:829-31. [Crossref] [PubMed]
- Christen S, Mendoza M, Gobet R, et al. Late ureteral obstruction after injection of dextranomer/hyaluronic acid copolymer. Urology 2014;83:920-2. [Crossref] [PubMed]
- Nseyo U, Mancini JG, Wiener JS. Symptomatic bilateral delayed partial ureteral obstruction after bilateral endoscopic correction of vesicoureteral reflux with dextranomer/hyaluronic acid polymer. Urology 2013;81:184-7. [Crossref] [PubMed]
- Vandersteen DR, Routh JC, Kirsch AJ, et al. Postoperative ureteral obstruction after subureteral injection of dextranomer/hyaluronic Acid copolymer. J Urol 2006;176:1593-5. [Crossref] [PubMed]
- Yankovic F, Swartz R, Cuckow P, et al. Incidence of Deflux(R) calcification masquerading as distal ureteric calculi on ultrasound. J Pediatr Urol 2013;9:820-4. [Crossref] [PubMed]
- Politano VA, Leadbetter WF. An Operative Technique for the Correction of Vesicoureteral Reflux. J Urol 2017;197:S94-100. [Crossref] [PubMed]
- Paquin AJ Jr. Ureterovesical anastomosis: a comparison of two principles. J Urol 1962;87:818-22. [Crossref] [PubMed]
- Glenn JF, Anderson EE. Distal tunnel ureteral reimplantation. J Urol 1967;97:623-6. [Crossref] [PubMed]
- Cohen SJ. The Cohen reimplantation technique. Birth Defects Orig Artic Ser 1977;13:391-5. [PubMed]
- Gil-Vernet JM. A new technique for surgical correction of vesicoureteral reflux. J Urol 1984;131:456-8. [Crossref] [PubMed]
- Marotte JB, Smith DP. Extravesical ureteral reimplantations for the correction of primary reflux can be done as outpatient procedures. J Urol 2001;165:2228-31. [Crossref] [PubMed]
- Lich R Jr, Howerton LW, Davis LA. Childhood urosepsis. J Ky Med Assoc 1961;59:1177-9. [PubMed]
- Gregoir W, Vanregemorter G. Congenital Vesico-Ureteral Reflux. Urol Int 1964;18:122-36. [PubMed]
- Palmer JS. Extravesical ureteral reimplantation: an outpatient procedure. J Urol 2008;180:1828-31; discussion 1831.
- Fung LC, McLorie GA, Jain U, et al. Voiding efficiency after ureteral reimplantation: a comparison of extravesical and intravesical techniques. J Urol 1995;153:1972-5. [Crossref] [PubMed]
- Austin JC, Cooper CS. Vesicoureteral reflux: surgical approaches. Urol Clin North Am 2004;31:543-57. x. [Crossref] [PubMed]
- Atala A, Kavoussi LR, Goldstein DS, et al. Laparoscopic correction of vesicoureteral reflux. J Urol 1993;150:748-51. [Crossref] [PubMed]
- Ehrlich RM, Gershman A, Fuchs G. Laparoscopic vesicoureteroplasty in children: initial case reports. Urology 1994;43:255-61. [Crossref] [PubMed]
- Janetschek G, Radmayr C, Bartsch G. Laparoscopic ureteral anti-reflux plasty reimplantation. First clinical experience. Ann Urol (Paris) 1995;29:101-5. [PubMed]
- Lakshmanan Y, Fung LC. Laparoscopic extravesicular ureteral reimplantation for vesicoureteral reflux: recent technical advances. J Endourol 2000;14:589-93; discussion 593-4. [Crossref] [PubMed]
- Sung J, Skoog S. Surgical management of vesicoureteral reflux in children. Pediatr Nephrol 2012;27:551-61. [Crossref] [PubMed]
- Bayne AP, Shoss JM, Starke NR, et al. Single-center experience with pediatric laparoscopic extravesical reimplantation: safe and effective in simple and complex anatomy. J Laparoendosc Adv Surg Tech A 2012;22:102-6. [Crossref] [PubMed]
- Castillo OA, Zubieta R, Yanez R. Laparoscopic surgery of vesicoureteral reflux: an experience in 42 patients with the Lich-Gregoir extravesical technique. Actas Urol Esp 2013;37:630-3. [Crossref] [PubMed]
- Canon SJ, Jayanthi VR, Patel AS. Vesicoscopic cross-trigonal ureteral reimplantation: a minimally invasive option for repair of vesicoureteral reflux. J Urol 2007;178:269-73; discussion 273. [Crossref] [PubMed]
- Tsai YC, Wu CC, Yang SS. Minilaparoscopic nerve-sparing extravesical ureteral reimplantation for primary vesicoureteral reflux: a preliminary report. J Laparoendosc Adv Surg Tech A 2008;18:767-70. [Crossref] [PubMed]
- Yeung CK, Sihoe JD, Borzi PA. Endoscopic cross-trigonal ureteral reimplantation under carbon dioxide bladder insufflation: a novel technique. J Endourol 2005;19:295-9. [Crossref] [PubMed]
- Chung PH, Tang DY, Wong KK, et al. Comparing open and pneumovesical approach for ureteric reimplantation in pediatric patients--a preliminary review. J Pediatr Surg 2008;43:2246-9. [Crossref] [PubMed]
- Lau CT, Lan LC, Wong KK, et al. Pneumovesical Ureteric Reimplantation in Pediatric Patients: An Intermediate Term Result. J Laparoendosc Adv Surg Tech A 2017;27:203-5. [Crossref] [PubMed]
- Bi Y, Sun Y. Laparoscopic pneumovesical ureteral tapering and reimplantation for megaureter. J Pediatr Surg 2012;47:2285-8. [Crossref] [PubMed]
- Soh S, Kobori Y, Shin T, et al. Transvesicoscopic ureteral reimplantation: Politano-Leadbetter versus Cohen technique. Int J Urol 2015;22:394-9. [Crossref] [PubMed]
- Bowen DK, Faasse MA, Liu DB, et al. Use of Pediatric Open, Laparoscopic and Robot-Assisted Laparoscopic Ureteral Reimplantation in the United States: 2000 to 2012. J Urol 2016;196:207-12. [Crossref] [PubMed]
- Peters CA. Robotically assisted surgery in pediatric urology. Urol Clin North Am 2004;31:743-52. [Crossref] [PubMed]
- Casale P, Patel RP, Kolon TF. Nerve sparing robotic extravesical ureteral reimplantation. J Urol 2008;179:1987-9; discussion 1990.
- Smith RP, Oliver JL, Peters CA. Pediatric robotic extravesical ureteral reimplantation: comparison with open surgery. J Urol 2011;185:1876-81. [Crossref] [PubMed]
- Kasturi S, Sehgal SS, Christman MS, et al. Prospective long-term analysis of nerve-sparing extravesical robotic-assisted laparoscopic ureteral reimplantation. Urology 2012;79:680-3. [Crossref] [PubMed]
- Akhavan A, Avery D, Lendvay TS. Robot-assisted extravesical ureteral reimplantation: outcomes and conclusions from 78 ureters. J Pediatr Urol 2014;10:864-8. [Crossref] [PubMed]
- Dangle PP, Shah A, Gundeti MS. Robot-assisted laparoscopic ureteric reimplantation: extravesical technique. BJU Int 2014;114:630-2. [Crossref] [PubMed]
- Grimsby GM, Dwyer ME, Jacobs MA, et al. Multi-institutional review of outcomes of robot-assisted laparoscopic extravesical ureteral reimplantation. J Urol 2015;193:1791-5. [Crossref] [PubMed]
- Herz D, Fuchs M, Todd A, et al. Robot-assisted laparoscopic extravesical ureteral reimplant: A critical look at surgical outcomes. J Pediatr Urol 2016;12:402.e1-9. [Crossref] [PubMed]
- Marchini GS, Hong YK, Minnillo BJ, et al. Robotic assisted laparoscopic ureteral reimplantation in children: case matched comparative study with open surgical approach. J Urol 2011;185:1870-5. [Crossref] [PubMed]
- Wang HH, Tejwani R, Cannon GM Jr, et al. Open versus minimally invasive ureteroneocystostomy: A population-level analysis. J Pediatr Urol 2016;12:232.e1-6. [Crossref] [PubMed]
- Kurtz MP, Leow JJ, Varda BK, et al. Robotic versus open pediatric ureteral reimplantation: Costs and complications from a nationwide sample. J Pediatr Urol 2016;12:408.e1-6. [Crossref] [PubMed]
- Boysen WR, Ellison JS, Kim C, et al. Multi-Institutional Review of Outcomes and Complications of Robot-Assisted Laparoscopic Extravesical Ureteral Reimplantation for Treatment of Primary Vesicoureteral Reflux in Children. J Urol 2017;197:1555-61. [Crossref] [PubMed]
- Peters CA, Woo R. Intravesical robotically assisted bilateral ureteral reimplantation. J Endourol 2005;19:618-21; discussion 621-2. [Crossref] [PubMed]
- Chan KW, Lee KH, Tam YH, et al. Early experience in robotic-assisted laparoscopic bilateral intravesical ureteral reimplantation for vesicoureteral reflux in children. J Robot Surg 2012;6:259-62. [Crossref] [PubMed]
- Singh-Grewal D, Macdessi J, Craig J. Circumcision for the prevention of urinary tract infection in boys: a systematic review of randomised trials and observational studies. Arch Dis Child 2005;90:853-8. [Crossref] [PubMed]
Cite this article as: Leung L, Chan IHY. Minimally invasive surgery in vesicoureteric reflux. Ann Laparosc Endosc Surg 2018;3:95.