内镜技术的优势
引言
自从腹腔镜微创手术在临床运用以来,在结直肠疾病的治疗方面越来越广。迄今,已有多项研究证实了腹腔镜手术在治疗结直肠良恶性疾病的安全性和有效性[1-6]。其中主要的优点有减少术后疼痛和麻醉药物的使用,减少术后住院时间,早期恢复肠功能,更快地恢复工作,降低术后切口疝的风险。在这篇文章中,我们特别关注在结肠手术中进行体内吻合的好处。
在减重手术中,从开放的Roux-en-y胃旁路术到腹腔镜下的Roux-en-y胃旁路术的实施,这是一个重大飞跃,由于腹腔镜胃旁路术过程中需要进行多次体内吻合,外科医生面临着一个较长的学习曲线,但如今,腹腔镜已成为胃旁路术乃至其他减重手术的标准操作[7,8]。腹腔镜结直肠手术近年来以来也取得了重大进展,有趣的是,对腹腔镜结直肠手术的描述依然包括足够大的切口以方便标本提取,使用手助腹腔镜技术,或联合开放入路进行盆腔手术。此外,许多外科医生在肠管离断后更倾向选择体外吻合来确保肠管连续性。
对于体外吻合的争议在于需要一个取出标本部位,但是取标本切口会给患者带来一定的负面影响,比如腹正中切口会增加切口疝的发生率,所以选择其他部位切口能让患者长期获益[9-11]。
与开放技术相比,微创系列的技术和方法改良了结直肠手术。术后住院时间、肠梗阻发生率、患者满意度等因素都可能会受到选择全腹腔镜技术进行体内吻合的影响。在本文中,我们将讨论体内吻合术其手术技术、优点及该技术与体外吻合术在术后结果方面的比较。
吻合口瘘
肠管吻合是每个结肠和直肠手术的关键部分,而手术中的吻合口瘘的发生率,据报道,回结肠为1%~3%,而结直肠吻合口的吻合口瘘率超过20%[12,13]。吻合口瘘是一种令人烦恼的并发症,这可能是外科医生不愿意在腹腔镜结直肠手术中进行体内吻合的一个影响因素,在这个关键处,许多人可能保持谨慎态度。此外,由于能够在特定的切口位置将肠管提出腹腔进行吻合,所以大多数外科医生认为没有必要进行体内吻合。
结肠切除术的开放手术和腹腔镜手术的吻合口瘘发生率相当[1,3]。尽管如上所述,还是有许多的研究,进行了体外吻合。为了比较体内与体外吻合,已经进行了多个小样本的研究,结果显示这两种技术之间的吻合口瘘的发生率没有统计学差异[14-17]。缺乏舒适的体内吻合器和缝合器可能是体内吻合技术发展相对缓慢的一个因素。但是,对经验丰富的外科医生来说,体内吻合发生吻合口瘘的概率和开放吻合相当。
切口疝
结肠切除术后切口疝是一种常见的并发症,可导致严重的后果,选择完全腹腔镜技术和体内吻合术可降低该风险,腹腔镜结直肠手术后的切口疝发生率可能高于30%[10]。显然,仅行腹腔镜手术并不能减轻切口疝的风险,这可能是由于外科医生选择通过腹正中线切口进行体外肠管吻合导致的。然而不幸的是,除非进行结直肠吻合术,否则腹正中线切口通常用于提出肠管进行体外吻合。腹正中线切口与其他切口相比,切口疝的发生率显著增加,尤其是和横切口比起来[9-11]。目前,正在开展一项由多机构参与的前瞻性研究,使用腹腔镜技术和机器人技术行右半结肠切除术,分别选择体内和体外吻合,研究术后切口疝的发生率。
经阴道或者经肛门等自然开口取出标本,可以减少切口疝的风险。而且这是完全腹腔镜手术,除了穿刺部位切口外没有其他切口。在选定的合适患者中,这些经自然腔道取出的方法已被证明是安全和可行的[18,19]。假如能放弃腹正中线或其他切口,对于任何接受腹腔镜结肠切除术的患者来说都是极有利的。
总的来说,避免术后切口疝的一个主要因素是对取出标本部位的评估,体内吻合时取标本位置可以考虑所有的切口部位,而体外吻合为了使其易于暴露手术野,限制了标本取出部位的选择。
手术部位感染
手术部位感染是结直肠手术中常见的问题,减少结肠切除术后的手术部位感染已成为重要工作。在清洁污染病例中保持无菌的习惯,如使用加盖的手术器械盒,在吻合术后更换手套和手术衣,以及使用切口保护器,这都与降低手术部位感染率有关。目前,体内和体外吻合的手术部位深部和浅表感染的发生率几乎相当[14,15,20]。
术后康复
腹腔镜结直肠切除术与患者术后短期预后的改善有关,腹腔镜手术可以减少术后肠梗阻,促进术后排气和减少住院时间。体内吻合在某些方面确实超越了体外吻合。无论单机构还是多机构研究经验都表明在肠功能恢复率和住院时间方面体内吻合较体外吻合有所改善,但并非在所有方面都能看到这种优势[20,21]。
技巧
顺蠕动性回结肠吻合术(图1)
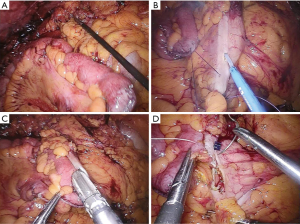
在吻合之前,在原计划横断位置切开肠系膜,回肠和结肠用线形闭合器分开,标本留待以后取出。回肠和结肠的切缘按照肠蠕动方向在右上腹位置对齐,将一条牵引线分别穿过系膜游离缘的结肠和回肠的闭合处。下一步,用超声刀切开肠管,将腹腔镜专用线性闭合器置入肠管中建立吻合部位的共同通道。肠切口通常使用可吸收缝合线缝合,不缩小吻合口,减少肠狭窄的发生。
逆蠕动性回结肠吻合术(图2)

当进行逆蠕动吻合术时,回肠和结肠要对准,使两条闭合线对齐。牵引缝线穿过两侧肠端闭合线的系膜游离缘侧,接着紧临牵引线切开肠管,同样使用线性闭合器来创建共同通道。凭外科医生喜好,可以用闭合器或腹腔镜下缝合关闭肠管。
结论
体内吻合术是一种安全可靠的技术,可为接受结肠和直肠手术的患者提供多种益处。实际操作就是将体外吻合技术在先进的腹腔镜设备的辅助下照搬到体内进行。最大的益处可能是术后切口疝的风险降低,目前对此正在进行一项前瞻性多中心研究。
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Michael J Stamos and Mehraneh Dorna Jafari) for the series “Laparoscopic Colon Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2018.12.08). The series “Laparoscopic Colon Surgery” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050-9. [Crossref] [PubMed]
- Braga M, Frasson M, Vignali A, et al. Laparoscopic vs. open colectomy in cancer patients: long-term complications, quality of life, and survival. Dis Colon Rectum 2005;48:2217-23. [Crossref] [PubMed]
- Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 2005;365:1718-26. [Crossref] [PubMed]
- Fleshman J, Branda ME, Sargent DJ, et al. Disease-free Survival and Local Recurrence for Laparoscopic Resection Compared With Open Resection of Stage II to III Rectal Cancer: Follow-up Results of the ACOSOG Z6051 Randomized Controlled Trial. Ann Surg 2018; [Epub ahead of print]. [Crossref] [PubMed]
- van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210-8. [Crossref] [PubMed]
- Jeong SY, Park JW, Nam BH, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 2014;15:767-74. [Crossref] [PubMed]
- Nguyen NT, Wolfe BM. Laparoscopic Versus Open Gastric Bypass. Semin Laparosc Surg 2002;9:86-93. [Crossref] [PubMed]
- Luján JA, Frutos MD, Hernández Q, et al. Laparoscopic Versus Open Gastric Bypass in the Treatment of Morbid Obesity: A Randomized Prospective Study. Ann Surg 2004;239:433-7. [Crossref] [PubMed]
- Singh R, Omiccioli A, Hegge S, et al. Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 2008;22:2596-600. [Crossref] [PubMed]
- Lee L, Mappin-Kasirer B, Sender Liberman A, et al. High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 2012;26:3180-5. [Crossref] [PubMed]
- DeSouza A, Domajnko B, Park J, et al. Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc 2011;25:1031-6. [Crossref] [PubMed]
- Eto K, Urashima M, Kosuge M, et al. Standardization of surgical procedures to reduce risk of anastomotic leakage, reoperation, and surgical site infection in colorectal cancer surgery: a retrospective cohort study of 1189 patients. Int J Colorectal Dis 2018;33:755-62. [Crossref] [PubMed]
- Masoomi H, Buchberg B, Dang P, et al. Outcomes of right vs. left colectomy for colon cancer. J Gastrointest Surg 2011;15:2023-8. [Crossref] [PubMed]
- Lee KH, Ho J, Akmal Y, et al. Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc 2013;27:1986-90. [Crossref] [PubMed]
- Hellan M, Anderson C, Pigazzi A. Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS 2009;13:312-7. [PubMed]
- Scatizzi M, Kroning KC, Borrelli A, et al. Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg 2010;34:2902-8. [Crossref] [PubMed]
- Shapiro R, Keler U, Segev L, et al. Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 2016;30:3823-9. [Crossref] [PubMed]
- McKenzie S, Baek JH, Wakabayashi M, et al. Totally laparoscopic right colectomy with transvaginal specimen extraction: the authors’ initial institutional experience. Surg Endosc 2010;24:2048-52. [Crossref] [PubMed]
- Akamatsu H, Omori T, Oyama T, et al. Totally laparoscopic sigmoid colectomy: a simple and safe technique for intracorporeal anastomosis. Surg Endosc 2009;23:2605. [Crossref] [PubMed]
- Vergis AS, Steigerwald SN, Bhojani FD, et al. Laparoscopic right hemicolectomy with intracorporeal versus extracorporeal anastamosis: a comparison of short-term outcomes. Can J Surg 2015;58:63-8. [Crossref] [PubMed]
- Trastulli S, Coratti A, Guarino S, et al. Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc 2015;29:1512-21. [Crossref] [PubMed]
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: Brady MT. The advantage of intracorporeal techniques. Ann Laparosc Endosc Surg 2019;4:12.