Technical tips concerning laparoscopic hepaticojejunostomy for choledochal cyst in children with a focus on secure anastomosis for small hepatic ducts
Introduction
Laparoscopic hepaticojejunostomy for choledochal cyst was first performed for adult patients in the late 1990s (1). Initially, cyst excision was performed laparoscopically, while hepaticojejunostomy was performed under direct vision through small laparotomy (2). Recently, all procedures, including cyst excision, Roux-Y anastomosis, and hepaticojejunostomy, in adult cases have come to be performed completely laparoscopically (3).
Laparoscopic surgery for choledochal cyst in children is also feasible, and many cases have been performed in Asian countries (4,5). In addition, single-incision laparoscopic surgery for choledochal cyst in small children has also been reported (6,7). In small infants, the organs are fragile and easily bleed, but dissection is not difficult because of the good visibility due to the small amount of fat tissue in abdominal cavity. However, laparoscopic hepaticojejunostomy for small hepatic ducts in children remains one of the most technically challenging aspects of such procedures. Pediatric surgeons require advanced needle-driving and suturing skills and must sometimes perform duct plasty for secure anastomosis (8,9).
We herein report a standardized procedure in our institution for performing laparoscopic hepaticojejunostomy for small hepatic ducts in children.
Patient selection and workup
Using preoperative imaging modalities, such as enhanced computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP) and drip infusion cholecysto-cholangiography-CT (DIC-CT), the type of common bile duct dilatation, type of pancreaticobiliary maljunction, length of common channel, presence or absence of protein plague, and variation of the right hepatic artery (positional relationship of hepatic duct) should be confirmed preoperatively. Regarding the timing for definitive operation, antenatal diagnosed cases should undergo the procedure electively at least three months after birth. However, a radical operation is technically feasible for patients over 3 kg in body weight (10).
Surgical position and port layout
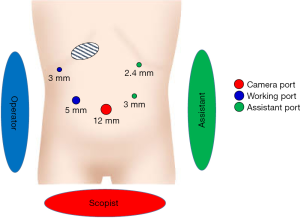
Under general anesthesia, older pediatric patients are placed in a broad base position. Small infants are placed in a supine position caudally on the operative bed so the operator can stand and manipulate the forceps at the end of the operation table. Our standard port placement is shown in Figure 1.
The umbilicus is opened through a 1.5-cm longitudinal incision, and a wound retractor (LAP PROTECTOR; Mini-mini; Hakko, Co., Ltd., Tokyo, Japan) is applied. A 5- or 10-mm 30° or 45° laparoscope is inserted through a special silicone cap (E·Z access for FF0504; Hakko, Co., Ltd.) to attach to the wound retractor. We routinely use a 10-mm rigid high-definition endoscope (KARLSTOZ, Tuttlingen, Germany). In most of the operative steps, the operator stands at the right side of the patient, except for during dissection of huge adhesive cysts. The assistant surgeon stands on the opposite side, and the camera assistant stands between the patient’s legs.
Pneumoperitoneum is established by CO2 insufflation at 8 mmHg. The CO2 flow is determined based on the patients’ size. Three additional trocars are inserted: one each at the right upper abdomen (3 mm, operator’s left hand), right side of the umbilicus (5 mm, operator’s right hand), and left lateral abdomen (3 mm, assistant’s left hand). A 2.4-mm percutaneous needle-type grasper (MiniLap®; Teleflex, Morrisville, NC, USA) is inserted at the left upper abdomen for gallbladder retraction, as shown in Figure 1.
The round ligament of the liver is elevated using 2-0 silk sutures through 19-G percutaneous needle ligature carrier insertion (LAPA-HER-CLOSURE, Hakko, Co., Ltd.) to provide vision of the inferior space of the liver. In general, the tissue around the lesion is likely to be wet or sometimes firm due to inflammation related to repeated cholangitis. Oozing hemorrhaging from the cyst wall in particular tends to hamper precise dissection. During the operative procedure, a suction device is also frequently used to suck out any superfluous discharge. Specialized small gauze for endoscopic surgery (TROXTM; Type D; Oosaki Medical, Nagoya, Japan) must be used for gentle suction. In this manner, a dry operative field can be maintained.
In cases of non-dilated pancreaticobiliary maljunction, the bile is sampled directly through percutaneous needle puncture, and the amylase level in the bile is measured. The amylase value will then determine whether hepaticojejunostomy or simple cholecystectomy should be performed.
Cyst dissection and excision
To obtain a sufficiently clear view of the hepatic portal region, the fundus of gallbladder is grasped with a percutaneous needle-type grasper (MiniLap®; Teleflex) and elevated toward the cranial direction. Using energy devices, such as a vessel sealing system (LigaSureTM Maryland; Medtronic plc, Minneapolis, MN, USA), a 3-mm Vessel sealer (JustRightTM 3-mm Vessel Sealing System; JustRight Surgical, LLC., Louisville, CO, USA), and an ultrasonically activated device (HARMONIC® HD 1000i Shears; Johnson & Johnson, New Brunswick, NJ, USA), along with 3.5-mm bipolar forceps (RoBi; KARLSTORZ), the cyst wall is carefully dissected. In cases of huge choledochal cyst, the bile is aspirated to obtain a posterior view of the cyst before dissection. Dissection of the posterior wall of the cyst is completely performed, and the cyst is taped. After taping of the cyst wall, the distal side of the cyst inside the pancreatic tissue is dissected. The pancreatic tissue is dissected around the cyst using sharp dissection. A metal clip (LIGAMAX5®; Johnson & Johnson) is applied at the distal side of the cyst as a landmark of transection.
Intraoperative cholangiography
The fundus of the gallbladder is dissected, and a catheter is inserted through the right upper 3-mm trocar or via the additional insertion of a 2-mm trocar (Mini Port; Medtronic plc). A catheter (CHOLANGIO-CATHETER; Hakko, Co., Ltd.) is ligated using an endoloop (ENDOLOOP® Ligature; Johnson & Johnson), and intraoperative cholangiography is performed. After measuring the distance between the landmark metal clip and the joint portion of the bile duct and pancreatic duct, additional dissection is performed as needed. The distal side of cyst is ligated just above the joint portion using 4-0 or 5-0 monofilament transfixing sutures (PDS® Plus; Johnson & Johnson), and a polymer clip (Weck® Hem-o-lok® Polymer Ligation System-Automatic; Teleflex) is additionally applied.
After transection of the distal side of the choledochal cyst, the posterior wall of the cyst is carefully dissected from the portal vein.
Preparation of the jejunal limb and Roux-en-Y anastomosis
Before performing Roux-en-Y anastomosis, the jejunum 30 cm distal from the ligament of Treitz is marked with crystal violet and grasped with forceps by the assistant surgeon under a laparoscopic view in order to maintain confirmation of the peristaltic direction. After the marked jejunum is grasped and the silicone cap detached (E·Z access for FF0504; Hakko, Co., Ltd.), the grasped jejunum is extracted through the wound retractor.
After verifying the vessels’ structure in the mesentery, the jejunum is divided using a linear stapler, usually approximately 30 cm distal from the ligament of Treitz. The marginal vessel is divided. If there is still strong tension so far, a branch of the jejunal artery and vein is divided after a clamping test using a temporary vessel clamper. The length of the jejunal limb is determined based on the patient’s body size (approximately 30–40 cm). Jejuno-jejunostomy is performed in a side-to-side fashion using a 35-mm linear stapler (Powered ECHELON FLEX®; Johnson & Johnson) or 25-mm linear stapler (JustRightTM 5-mm Stapler; JustRight Surgical, LLC), and the entry hole is closed by hand-sewing in the full-thickness layer using 5-0 monofilament sutures (PDS® Plus; Johnson & Johnson). The mesentery gap that results from the jejuno-jejunostomy is also closed by hand-sewing.
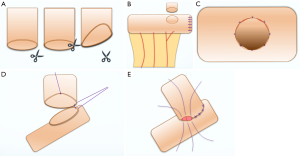
Finally, a small anastomotic hole for the subsequent hepaticojejunostomy is made at the end of the jejunal limb. The size of the anastomotic hole is determined based on the size of the hepatic duct. The anastomotic hole is positioned not just at the anti-mesenteric side but also slightly anterior on the abdominal side to ensure good visualization during hepaticojejunostomy After making the anastomotic hole, the mucosa and the serosa are approximate using 6-0 monofilament (PDS® Plus; Johnson & Johnson) interrupted sutures. This procedure is important for performing membrane-to-membrane hepaticojejunostomy of a small hepatic duct. Because deciding on the position for Roux-en-Y anastomosis under laparoscopy can be difficult in infants and small children, it is routinely done under direct vision while measuring the distance accurately and stretching the intestine outside of the abdominal wall.
Duct-plasty and hepaticojejunostomy
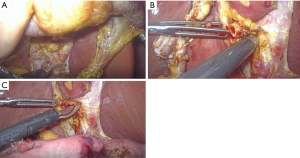
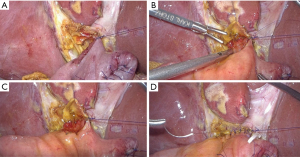
There is a risk of anastomotic stricture after hepaticojejunostomy in patients with a small hepatic duct. In our standardized method, the hepatic duct is resected at the common hepatic duct level above the cyst (Figure 2A). The small hepatic duct is enlarged using a diagonal cut up the left side of the hepatic duct (in the 3 o’clock direction) (Figure 2B,C). We do not cut the right side of the hepatic duct in order to avoid injuring the posterior branch. For the cutting device, we use fine scissors (Mini Endocut; Microline Surgical, Beverly, MA, USA). Hemostasis at the cutting edge of the hepatic duct is minimum in order to prevent thermal injury of the hepatic duct. At the start of hepaticojejunostomy, we usually lay down stay sutures at the left side of the hepatic duct (in the 3 o’clock direction). After stay suture using 5-0 monofilament (PDS® Plus; Johnson & Johnson) intracorporeal knot tying is made at left side of hepatic duct, the long tail of the suture is suspended by the needle device (LAPA-HER-CLOSURE, Hakko, Co., Ltd.) insertion at the left upper abdomen (Figure 3A). After stay sutures are laid, the posterior wall is sutured using interrupted 6-0 absorbable monofilament (PDS® Plus; Johnson & Johnson) intracorporeal knot tying (Figure 3B). In order to obtain stable visualization and perform secure membrane-to-membrane anastomosis, the anterior wall of the hepatic duct is also suspended using 5-0 absorbable monofilament (PDS® Plus; Johnson & Johnson) from outside of the body (Figure 3C). After finishing the posterior wall anastomosis, the anterior wall is sutured as same fashion of 6-0 monofilament (PDS® Plus; Johnson & Johnson) intracorporeal knot tying. The suspending sutures is removed after half of the anterior wall of the anastomosis is finished. Before finishing the anterior wall of anastomosis, only needle-driving is performed for the final three sutures (Figure 3D). And then knot tying is performed to finish the hepaticojejunostomy. This technique helps avoid the risk of the involvement of posterior wall needle-driving during anterior wall anastomosis because of confirming the lumen of the hepatic duct and mucosal layer of the anastomotic hole of jejunum. Anastomosis is completely performed without stent insertion.
Post-operative management
A 10- or 15-Fr closed-type drainage tube with continuous aspiration is placed behind the hepaticojejunostomy. The amylase levels of the discharge in the tube are measured on the 1st and 3rd postoperative days. If no abnormal elevation of the amylase levels or cloudiness is noted in the discharge, the tube is removed on the 4th postoperative day. Drinking water is started on the 3rd or 4th postoperative day, and soft meals are started on the 5th postoperative day. Patients are discharged from the hospital on the 7th–9th postoperative day if no complications are noted.
Pitfalls and strategies for managing difficult situations
Duct plasty and confirmation of the lumen for anastomosis are important points associated with pitfalls in hepaticojejunostomy of small hepatic ducts in children. Our cutting method and anastomotic procedure are effective and useful for performing hepaticojejunostomy, even for surgeons in training (Figure 4). However, pediatric surgeons must endeavor to acquire precise needle-driving and stable knot-tying techniques.
Acknowledgments
We thank Mr. Brian Quinn for his comments and help with the manuscript.
Funding: This study was supported by: Research Grant from President’s Discretionary Expenses of our University, Research Grant from The UBE Foundation, Research Grant from Kawano Masanori Memorial Public Interest Incorporated Foundation for Promotion of Pediatrics, Research Grant from Tateishi Science and Technology Foundation, Research Grant from Mitsui Life Social Welfare Foundation, Research Grant from the Kurata Grants of the Hitachi Global Foundation, Research Grant from Foundation for Promotion of Cancer Research, Research Grant from Foundation for Shinnihon Zaidan, Research Grant from Suzuken Memorial Foundation, Research Grant from Princess Takamatsu Research Foundation, Research Grant from the Japanese Society for Medical and Biological Engineering.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kenneth K. Y. Wong and Patrick Ho Yu Chung) for the series “Paediatric Minimally Invasive Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.02.03). The series “Paediatric Minimally Invasive Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shimura H, Tanaka M, Shimizu S, et al. Laparoscopic treatment of congenital choledochal cyst. Surg Endosc 1998;12:1268-71. [Crossref] [PubMed]
- Tanaka M, Shimizu S, Mizumoto K, et al. Laparoscopically assisted resection of choledochal cyst and Roux-en-Y reconstruction. Surg Endosc 2001;15:545-52. [Crossref] [PubMed]
- Aly MYF, Mori Y, Miyasaka Y, et al. Laparoscopic surgery for congenital biliary dilatation: a single-institution experience. Surg Today 2018;48:44-50. [Crossref] [PubMed]
- Qiao G, Li L, Li S, et al. Laparoscopic cyst excision and Roux-Y hepaticojejunostomy for children with choledochal cysts in China: a multicenter study. Surg Endosc 2015;29:140-4. [Crossref] [PubMed]
- Liem NT, Pham HD. Early and intermediate outcomes of laparoscopic surgery for choledochal cysts with 400 patients. J Laparoendosc Adv Surg Tech A 2012;22:599-603. [Crossref] [PubMed]
- Diao M, Li L, Dong N, et al. Single-incision laparoscopic Roux-en-Y hepaticojejunostomy using conventional instruments for children with choledochal cysts. Surg Endosc 2012;26:1784-90. [Crossref] [PubMed]
- Son TN, Liem NT, Hoan VX. Transumbilical laparoendoscopic single-site surgery with conventional instruments for choledochal cyst in children: early results of 86 cases. J Laparoendosc Adv Surg Tech A 2014;24:907-10. [Crossref] [PubMed]
- Tanaka Y, Tainaka T, Sumida W, et al. Introduction of resection of intrahepatic bile duct stenosis-causing membrane or septum into laparoscopic choledochal cyst excision. Pediatr Surg Int 2018;34:1087-92. [Crossref] [PubMed]
- Tanaka Y, Tainaka T, Sumida W, et al. The efficacy of resection of intrahepatic bile duct stenosis-causing membrane or septum for preventing hepatolithiasis after choledochal cyst excision. J Pediatr Surg 2017;52:1930-3. [Crossref] [PubMed]
- Diao M, Li L, Cheng W. Timing of surgery for prenatally diagnosed asymptomatic choledochal cysts: a prospective randomized study. J Pediatr Surg 2012;47:506-12. [Crossref] [PubMed]
Cite this article as: Ieiri S, Murakami M, Baba T, Harumatsu T, Yamada K. Technical tips concerning laparoscopic hepaticojejunostomy for choledochal cyst in children with a focus on secure anastomosis for small hepatic ducts. Ann Laparosc Endosc Surg 2019;4:20.