Is there any role for single-port right colectomy for cancer?
Background
The single port laparoscopic technique was first described in 1999 by Bresadola (1) for cholecystectomy. Subsequently in 2008 the first single port right hemicolectomy was reported by Bucher (2). Since then, many studies have reported that colorectal single incision laparoscopic surgery (SILS) is feasible and safe as multiport laparoscopic surgery (MPLS) in selected patients (3-8). It is postulated that single port access as well as NOTES provides better esthetic benefit, less postoperative pain and shorter hospitalization compared to standard laparoscopic procedures. The main disadvantage is longer operative time, difficulty in instrument triangulation, a learning curve and in addition cross handling instruments through two channels of a multi-instrument access port is necessary to compensate for the technical difficulties associated with SILS. However, there is no clear evidence supporting the benefits of SILS over MPLS in regards to better cosmetic outcome, less postoperative pain and shorter hospital stay. There are very few studies that have investigated the oncological outcome after SILS (5,9).
Indications and contraindications
The laparoscopic approach either multiple incisions or single incision approach to colon resections has generally become the preferred method over open surgery for nearly all colorectal surgical procedures. There are no absolute contraindications to laparoscopic colon procedures. However, extra attention should be taken to patients with a history of previous abdominal surgeries, cardiopulmonary comorbidities, obese patients, and pregnant patients where the use of laparoscopy is more controversial.
Preoperative assessment
Single incision laparoscopic right colon resection candidates need to be preoperatively evaluated like any other patient undergoing colon resection. All patients should be fully informed of the details of the operative procedure and the possible need for additional ports or conversion to open laparotomy if operation is difficult. We recommend reviewing all imaging studies and colonoscopy reports and tattooing early tumors prior to the procedure.
Even though the literature does not demonstrate clear cut superiority of bowel prep and oral antibiotics prior to elective colon resections; a combined mechanical bowel prep and oral antibiotics is preferred prior to surgery. The latter has shown improved surgical site infection rates among all types of colon resections and a decreased anastomotic leak (10).
Surgical technique
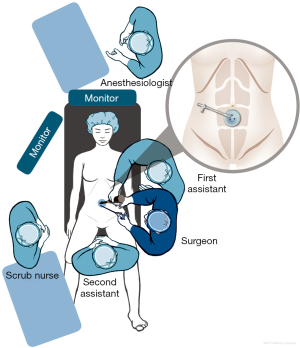
The procedure is done under general anesthesia and at least two monitors on both sides of the patient is preferred. We prefer to secure the patient to the operating table with arms in a tucked position allowing for safe and frequent position changes during the procedure. Some surgeons position the patient in a supine position throughout the procedure. We prefer a Lloyd Davis or modified lithotomy position using levator stirrups. The surgeon is usually positioned to the left of the patient and the first assistant is usually to the right of the surgeon. The second assistant is usually to the right of the patient or in between the legs if a modified lithotomy position is used. The scrub nurse provides instruments left of the surgeon (Figure 1).
A midline incision is performed above and below the umbilicus and to the left approximately 3 to 6 cm in length, followed by dissection of the layers of the abdominal wall into the peritoneal cavity. There are many multi-channel access devices from different brands that are now commercially available and any one of them can be used. A Covidien (one 12-mm channel, two 5-mm channels, and a separate channel providing CO2 insufflation can be used temporarily for a fourth instrument), Tri-Port Access System (Olympus), EZ Access (Hakko, Nagano, Japan) (one 12-mm channel and two 5-mm channels, or Octo Port (Dalim Medical, Seoul, Korea) (two 12-mm channels and two 5-mm channels (3,4,6,7).
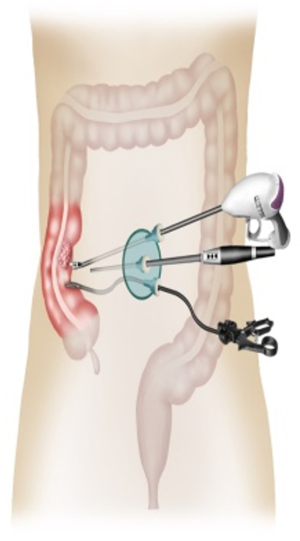
The instruments that are used in this procedure are the same instruments that are used in conventional laparoscopic right colon resection (Figure 2). Various energy devices, electric knife or coagulation shears can be used depending on the surgeon’s preference through the two channels of the SILS port. A 5-mm atraumatic intestinal forceps is used to prepare the operative field for vision and the other hand uses the preferred energy device to perform surgery. The assistant handles the laparoscope through one channel of the SILS port to create a working view.
The patient is put in Trendelenburg and left side down position and dissection is usually carried from medial to lateral exposing to ileocolic pedicle and right colonic vessels, with the help of atraumatic forceps held with the left hand and using the energy devices in the right hand.
Retroperitoneal plane dissection is continued extending laterally and deep into the right colon above Gerota’s fascia and medially by detaching retroperitoneal adhesions of the duodenum. The colon is mobilized along the line of Told until the hepatic flexure and then the transverse colon is mobilized. The omentum attached to the colon is divided by energy devices. The operator performs the procedure while parallel or cross-handling the instruments. After a complete Ileocolic dissection and checking for hemostasis an extra corporeal transection and anastomoses or an intra-corporeal transection and anastomosis can be performed depending on operator preference and technical skills. An articulated laparoscopic linear stapler can be inserted directly to one channel of the SILS port and vertical transection of the terminal ileum and proximal colon can be accomplished. The specimen is extracted through the SILS port. If an extracorporeal anastomosis is to be performed after removing the SILS port, a wound protector should be placed at the incision site and an extracorporeal functional side-to-side or end-to-side anastomosis is accomplished using conventional staplers or a hand sewn anastomosis. Sometimes additional ports can be needed especially if there are dense adhesions or excessive visceral fat or a tight working space. Postoperatively we utilize enhanced recovery protocol with the patient starting on a liquid diet on postop day zero.
Outcomes
It has been established that single port laparoscopic surgery is feasible and safe for right hemicolectomy. Skin incision lengths vary on average between 3 to 8 cm depending on the device used and the size of the tumor. Complication rates vary between 9% and 31.5% for minor complications and 3.2% to 9.6% for major complications in the literature (4,8,11,12). In a meta-analysis the overall rates of postoperative morbidity after SILS and MPLS for colorectal cancer are 14.1% and 13.4% respectively (13). There are three randomized controlled trials comparing single port colectomy to multi-port colectomy in colorectal neoplasms in the literature (4,6,7). These studies reveal that it is possible to perform an oncological surgical procedure; the total number of harvested lymph nodes, tumor free margins and length of specimen are comparable to MPLS. In regards to recurrence rates or disease free survival no outcome is reported. The largest trial is still ongoing and the authors will report 5-year disease free survival at the termination of the follow up (4).
In addition to limited instrument movement and poor ergonomics the maintenance of SILS skills is different from conventional a laparoscopic surgery and it is more difficult to maintain. When operative time, conversion, reoperation, perioperative complications and postoperative morbidity and mortality as well as 30-day readmission and oncological outcome is comparable between MPLS and SILS, outcomes are similar in published series.
Well-designed randomized controlled trials are needed to assess long-term outcomes in oncologic right colon resection in SILS.
The European Association for Endoscopic Surgery (EAES) issued a consensus statement stating “considering the increased direct costs (devices, instruments and operating time) of the SILS procedure and the prolonged learning curve wider acceptance of the procedure should be supported only after demonstration of clear benefits”. The Society (EAES) did not specify right colons but for all colon surgery their recommendation was: in selected patients (<T4 tumors, tumors <5 m in size, BMI <35, no previous abdominal surgery) SILS colonic resection could be offered to patients as an equally safe and effective alternative compared to multiport colonic surgery with comparable histological surrogate outcome. The grade of recommendation is weak (14).
Conclusions
SILS is feasible and safe for right hemicolectomy. There is no clear evidence supporting the benefit of SILS over MPLS in regards to better cosmetic outcome, less postoperative pain and shorter hospital stay. Even though, perioperative complications and short-term oncologic outcome is comparable between SILS and MPLS; no data is available in regards to long-term recurrence rates or disease free survival for right colon cancer. Well-designed randomized controlled trials are needed to assess long-term outcomes in oncologic right colon resection in SILS.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Roberto Bergamaschi and Mahir Gachabayov) for the series “Right Colon Cancer Surgery: Current State” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.05.08). The series “Right Colon Cancer Surgery: Current State” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bresadola F, Pasqualucci A, Donini A, et al. Elective transumbilical compared with standard laparoscopic cholecystectomy. Eur J Surg 1999;165:29-34. [Crossref] [PubMed]
- Bucher P, Pugin F, Morel P. Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis 2008;23:1013-6. [Crossref] [PubMed]
- Kim CW, Hur H, Min BS, et al. Oncologic outcomes of single-incision laparoscopic surgery for right colon cancer: A propensity score-matching analysis. Int J Surg 2017;45:125-30. [Crossref] [PubMed]
- Watanabe J, Ota M, Fujii S, et al. Randomized clinical trial of single-incision versus multiport laparoscopic colectomy. Br J Surg 2016;103:1276-81. [Crossref] [PubMed]
- Yamamoto M, Asakuma M, Tanaka K, et al. Clinical impact of single-incision laparoscopic right hemicolectomy with intracorporeal resection for advanced colon cancer: propensity score matching analysis. Surg Endosc 2019; [Epub ahead of print]. [Crossref] [PubMed]
- Poon JTC, Cheung CW, Fan JKM, et al. Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc 2012;26:2729-34. [Crossref] [PubMed]
- Huscher CG, Mingoli A, Sgarzini G, et al. Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early results of a randomized prospective study. Am J Surg 2012;204:115-20. [Crossref] [PubMed]
- Chen WTL, Chang SC, Chiang HC, et al. Single-incision laparoscopic versus conventional laparoscopic right hemicolectomy: a comparison of short-term surgical results. Surg Endosc 2011;25:1887-92. [Crossref] [PubMed]
- Papaconstantinou HT, Thomas JS. Single-incision laparoscopic colectomy for cancer: assessment of oncologic resection and short-term outcomes in a case-matched comparison with standard laparoscopy. Surgery 2011;150:820-7. [Crossref] [PubMed]
- Midura EF, Jung AD, Hanseman DJ, et al. Combination oral and mechanical bowel preparations decreases complications in both right and left colectomy. Surgery 2018;163:528-34. [Crossref] [PubMed]
- Ramos-Valadez DI, Patel CB, Ragupathi M, et al. Single-incision laparoscopic right hemicolectomy: safety and feasibility in a series of consecutive cases. Surg Endosc 2010;24:2613-6. [Crossref] [PubMed]
- Kirk KA, Boone BA, Evans L, et al. Analysis of outcomes for single-incision laparoscopic surgery (SILS) right colectomy reveals a minimal learning curve. Surg Endosc 2015;29:1356-62. [Crossref] [PubMed]
- Hoyuela C, Juvany M, Carvajal F. Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: A systematic review and meta-analysis. Am J Surg 2017;214:127-40. [Crossref] [PubMed]
- Morales-Conde S, Peeters A, Meyer YM, et al. European association for endoscopic surgery (EAES) consensus statement on single-incision endoscopic surgery. Surg Endosc 2019;33:996-1019. [Crossref] [PubMed]
Cite this article as: Alzghari T, Ozuner G. Is there any role for single-port right colectomy for cancer? Ann Laparosc Endosc Surg 2019;4:54.