Laparoscopic D3 dissection and complete mesocolic excision for right-sided colon cancer based on surgical anatomy
Introduction
Colorectal cancer (CRC) is one of the major leading cause of cancer-related death worldwide (1). In Japan, CRC is common cancer and the second leading cause of death. In addition to total mesenteric excision (TME) for rectal cancer, D3 dissection [central vascular ligation (CVL)] and complete mesocolic excision (CME) are two critical aspects of right hemicolectomy for right-sided colon cancer (RCC) (2-4). With regard to CME, Kanemitsu et al. reported the importance of gaining a preoperative understanding of vessel patterns for D3 dissection around the root of the dominant artery for RCC. Specifically, the procedure should start with dissection from the left edge of the superior mesenteric artery (SMA) using a medial approach with non-touch isolation, and proceed around the root of the dominant vessel from the ileocolic artery (ICA) in the right transverse colon and from the middle colic artery (MCA) in the left to middle transverse colon. Dissection should continue up to the inferior edge of the pancreas. In that report, the authors retrospectively demonstrated excellent long-term outcomes of D3 dissection in right hemicolectomy using an open surgery approach (5). Adequate lymph node dissection is also important for accurate staging and therapy. The laparoscopic approach for stage II/III RCC is becoming more common and may improve short- and long-term outcomes.
Nonetheless, D3 dissection for RCC is a difficult procedure due to variations in dominant vessels. For example, inflow veins to the surgical trunk may take anatomically distinct pathways. An understanding of vessel patterns is thus essential for D3 dissection around the surgical trunk and root of the MCA for RCC.
Here we describe a safe procedure for laparoscopic right hemicolectomy using a caudal approach with D3 dissection along the dominant artery for RCC.
Operative technique
Positioning and port placement
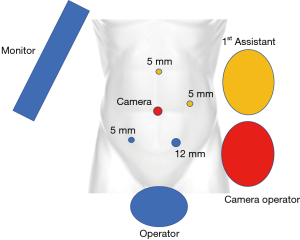
The patient was placed in the lithotomy position using the bean bag moldable device under general anesthesia. As first step, Kii balloon blunt tip (Applied Medical, Rancho Santa Margarita, CA, USA) was placed using an open approach, and then the abdominal cavity was explored with a 10-mm 30-degree laparoscope (Stryker, USA). Pneumoperitoneum was induced and maintained at 10 mmHg with carbon dioxide gas. Three 5-mm ports and a 12-mm port (ENDOPATH Xcel 5 mm & 12 mm, Ethicon Endo-Surgery, Cincinnati, OH, USA) were inserted into the abdominal cavity (Figure 1). Since the terminal ileum, right colon, and transverse colon were attached to the retroperitoneum, they were mobilized using Harmonic HD shears (Ethicon Endo-Surgery, Cincinnati, OH, USA). A 5-cm abdominal midline incision was made through umbilicus and a wound retractor (ALEXIS wound retractor S, Applied Medical, Santa Margarita, CA, USA) was introduced for extracorporealization of the colon.
Operative details
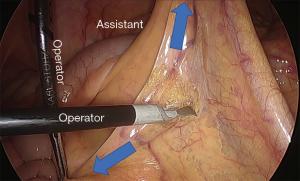
Identifying the ileocolic pedicle and caudal approach (Figure 2)
By gently stretching the ileocecal junction, the ileocolic pedicle was easily identified. The caudal approach was initiated by grasping the ileocolic pedicle and continued by dissecting the ventral surgical plane of fusion fascia. The duodenum and pancreas were automatically and gently left on the dorsal plane of the dissection layer.
D3 dissection (CVL) procedure (Figure 3)

D3 dissection was started from the left edge of the SMA using a medial approach with non-touch isolation. We dissected around the root of the dominant vessel from the ICA in the right transverse colon and from the MCA in the left to middle transverse colon, and continued the dissection up to the inferior edge of the pancreas.
Mobilization of the right colon (Figure 4)

After D3 dissection, the ileal and lateral colonic attachments were divided starting at the cecum and moving cranially to the hepatic flexure. First, the greater omentum was divided from the transverse colon and then gastro-colic ligament was divided. After the hepato-colic ligament was divided, the right-side colon was completely mobilized.
Extraction and extracorporeal anastomosis
The small abdominal incision should be extended to around 5 cm and followed by placement of the wound protector. The ileocolic junction was grasped using a Babcock clamp externally and exteriorized. Caution should be exercised so as not to tear or twist the mesentery. After ileum and transverse colon mesentery extraction, linear staplers (powered ECHELON FLEXTM ENDOPATH® stapler, 60 mm stapler, Ethicon Endo-Surgery, Inc., Cincinnati, Ohio, USA) were used to divide the ileum and transverse colon. Functional end-to-end anastomosis (FEEA) was performed with linear staplers and the crotch of the side-to-side anastomosis was buttressed with two 4-0 PDS stitches (Ethicon, Somerville, NJ, USA).
Conclusions
Laparoscopic D3 dissection and CME for RCC based on surgical anatomy are useful and feasible procedures which may improve surgical outcomes.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2019.09.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet 2014;383:1490-502. [Crossref] [PubMed]
- Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis 2009;11:354-64; discussion 364-5. [Crossref] [PubMed]
- Kotake K, Mizuguchi T, Moritani K, et al. Impact of D3 lymph node dissection on survival for patients with T3 and T4 colon cancer. Int J Colorectal Dis 2014;29:847-52. [Crossref] [PubMed]
- West NP, Hohenberger W, Weber K, et al. Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 2010;28:272-8. [Crossref] [PubMed]
- Kanemitsu Y, Komori K, Kimura K, et al. D3 Lymph Node Dissection in Right Hemicolectomy with a No-touch Isolation Technique in Patients With Colon Cancer. Dis Colon Rectum 2013;56:815-24. [Crossref] [PubMed]
Cite this article as: Moritani K, Kanemitsu Y, Takamizawa Y, Shida D, Tsukamoto S, Sakamoto R. Laparoscopic D3 dissection and complete mesocolic excision for right-sided colon cancer based on surgical anatomy. Ann Laparosc Endosc Surg 2019;4:99.