Surgery of the pancreatic cystic echinococcosis: a case report
Introduction
Cystic Echinococcosis (CE) is a continuing serious public health problem in endemic area (1).The two most frequent locations are liver and lung (1). Extrahepatic and lung CE are rare (2). The problems raised by echinococcosis vary according to its location (2). Diagnosis and management of each location have their particularities (2). The prevalence of pancreatic cystic echinococcosis (PCE) is ranging between 0.2% and 0.6% (3). The diagnosis of PCE is easy when it is associated with liver CE; it becomes difficult when PCE was isolated simulating other diagnosis (3). Ultrasonography and magnetic resonance imaging are very useful to confirm diagnosis (3). The therapeutic decision depends on the PCE location: conservative surgery for the head of the pancreas and radical surgery for body and/or tail of the pancreas (3). Medical treatment (albendazole) should be prescribed one week before surgery and two months during the postoperative period (3).
This article aimed to present a case of isolated PCE that simulated a mucinous cyst. The diagnosis of PCE was retained intraoperatively. A radical surgery was performed.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/ales-2019-11).
Case presentation
In this video article, we presented the case of a 55-year-old man, who had previously two episodes of acute pancreatitis on August 2016 and January 2017 that favorably managed with medical treatment in another center. On February 22nd, 2017, he was admitted with the diagnosis of pancreatic pseudocyst. Abdominal exam was normal.
Computed Tomography scan (CT scan) dated on February 23rd, 2017 revealed a dilation of Wirsung duct accompanied with a multiloculated cyst localized in the body and tail of the pancreas. Common bile duct was normal. The patient complained during hospitalization of a third episode of acute pancreatitis that was confirmed by lipasemia level at 20 folds of normal value. Ranson bio clinical score was one. He had a well recovery after one week with normal lipasemia.
Pancreatic Magnetic Resonance Imaging (Pancreatic MRI) on March 6th, 2017 showed the same description, however diagnosis of mucinous cyst of the pancreas was raised. Final decision was “wait and watch” with a planned CT scan one month later. The patient left hospital on March 7th, 2017.
Three other CT Scans showed the same imaging with a discrete increase of the multiloculated cysts size, associated with venous collateral circulation and multiples strictures of Wirsung duct (Figure 1). Another pancreatic MRI showed unchanged lesions (Figure 2).
On June 12th, 2017, the patient was Re hospitalized for a fourth episode of acute pancreatitis. The Staff Decision (June 12th, 2017) concluded that the case concerned a 55 year-old-male, ASA1, who had previously four episodes of acute pancreatitis, presented a pancreatic cyst evoking an Intra ductal Papillary Mucinous Neoplasm. Another CT scan was performed on October 26th, 2017 and then spleno-pancreatectomy was planned. He was operated on November 11th, 2017.
Operative technique—video comment (Video 1)
- Positioning of the patient The patient was on supine position. Surgeon was on the right of the patient and first aid on the left. Bi subcostal incision was performed.
- Exposure of the pancreas
— Opening of the lesser sac The gastro-colic ligament was sectioned with electrofusion energy device. The cystic tumor was easily identified when lesser sac was entered. The stomach was mobilized from the antrum. - Development of the retro
- pancreatic plane- splenic vein The retro pancreatic space was opened at the inferior border of the pancreas. The spleen was mobilized after section of peritoneal attachments (sustentaculum lienis). Pitfalls: At this step, an intraoperative ultrasonography should have been performed to identify the content and the limits before positioning the stapler. - Completion of mobilization, stapling of the pancreas: After complete mobilization of the pancreas, cyst was incidentally opened; a daughter vesicle irrupted into the peritoneal cavity and was immediately removed. Afterwards, the diagnosis of primary cystic echinococcosis of the pancreas was retained. The stapler was positioned on the body of the pancreas and when surgeon started to transect the pancreas using a gentle compression to avoid tissue damage, a frank rupture of the cyst occurred and several daughter cysts went into peritoneal cavity limited to the lesser sac. All these daughter vesicles were aspirated and the content was evacuated. A clamp was positioned on the pancreatic head’s distal margin and Irrigation with hypersaline water was performed to avoid a further dissemination. Pitfalls: A protection with soaked mesh in hypersaline solution should have been useful to prevent peritoneal dissemination.
- Splenectomy and distal pancreatectomy via bi
- subcostal incision: A distal pancreatectomy associated to splenectomy was performed. No other incident occurred. - Looking for daughter vesicle in the remnant Wirsung duct of the head: The remnant Wirsung duct of pancreatic head was dilated. The operator checked for daughter vesicles in the remnant Wirsung duct. No daughter vesicle found. Separate sutures were used to close the pancreatic transection. A drain was placed in the splenic bed and another in front of pancreatic transection.
Outcome
The post-operative course was uneventful. The two drains provided a serous and hematic liquid with an average of 33 mL/day. On the fifth postoperative day, amylase in the drainage liquid was at normal level. He was discharged on postoperative day 7.
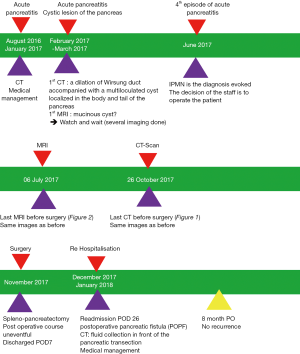
He was re admitted in the surgical department on postoperative day 26 with the diagnosis of postoperative pancreatic fistula (POPF). Physical exam showed a patient with a good status health. No organ failure was noticed. The sub costal incision healed, however there was a POPF raised through the orifice of the previous drainage providing a serous liquid with an average of 50ml/day. CT scan, performed at admission, showed a fluid collection in front of the pancreatic transection communicating the Wirsung duct with skin. This POPF was medically managed with favorable aftermath as confirmed by CT scan on the 23rd day after re admission. The patient was discharged on January 18th, 2018. No Anti cystic echinococcosis drug was prescribed. After a follow up of eight months, no recurrence was observed (Figure 3: case report timeline figure).
Conclusions
In this video article, we presented a case of isolated PCE that simulated a mucinous cyst. An epigastric pain was the main symptom evoking an acute pancreatitis regarding the high level of lipasemia. The Computed Tomographic scan and magnetic resonance imaging were in favor of pancreatic cyst evoking an Intra ductal Papillary Mucinous Neoplasm. The diagnosis of PCE located in the body and tail was recognized intraoperatively. A spleno distal pancreatectomy (radical surgery) was performed.
The main “take away” lesson from this case is that diagnosis of PCE is difficult when PCE was isolated simulating other diagnosis. On the other hand, diagnosis of PCE becomes easy when it is associated with liver CE. The therapeutic decision depends on the PCE location: conservative surgery for the head of the pancreas and radical surgery for body and/or tail of the pancreas. Surgeons should take care for the dissemination of echinococcosis.
The limitations of this report were three: (I) an intraoperative ultrasonography should have been performed to identify the content and the limits before positioning the stapler; (II) a protection with soaked mesh in hypersaline solution should have been useful to prevent further peritoneal dissemination and (III) anti cystic echinococcosis drug was indicated during the postoperative course for three months.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/ales-2019-11
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-2019-11). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was waived as patient identification and information remained anonymous for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dziri C. Hydatid disease--continuing serious public health problem: introduction. World J Surg 2001;25:1-3. [Crossref] [PubMed]
- Mzabi R, Dziri C. Les échinococcoses extrahépatiques: diagnostic et traitement Rev Prat 1990;40:220-4. [Extrahepatic echinococcosis: diagnosis and treatment]. [PubMed]
- Dziri C, Dougaz W, Bouasker I. Surgery of the pancreatic cystic echinococcosis: systematic review. Transl Gastroenterol Hepatol 2017;2:105. [Crossref] [PubMed]
Cite this article as: Dziri C, Bokal Z, Dougaz W, Mannai S. Surgery of the pancreatic cystic echinococcosis: a case report. Ann Laparosc Endosc Surg 2020;5:30.