Abdominal wall surgery in bariatric patients
Introduction
Obesity is one of the main factors for the development of incisional hernia. In addition, surgical repair of ventral hernias (VHs) in obese patients is clearly associated with a higher rate of complications and recurrences (1). Among the different complications that may occur after ventral hernia repair (VHR), we can find wound infection, evisceration, thromboembolic events or recurrence. Increased abdominal circumference, amount of fatty tissue, type 2 diabetes and increase of intra-abdominal pressure are obesity-related factors that clearly influence the higher number of infections and recurrence rate in these patients.
Abdominal wall surgery is one of the most frequent procedures performed by surgeons in our hospitals. Nowadays there is a high prevalence of obesity, which makes this surgery increasingly challenging. Preoperative optimization of patients is paramount to decrease the risk of postoperative complications and include stop smoking, improve the nutritional status and lose weight among others.
Certainly, one of the key points included in the optimization of patients that improve the results of this abdominal wall surgery is preoperative weight loss. In most cases, it is recommended to defer elective surgery until achieving an optimal weight, assuming the risk of increasing the defect, which will make the procedure more difficult in the future, or the risk of strangulation.
Based on these issues, the question that arises is if we should offer to these patients a bariatric procedure and differ the hernia surgery, or if the two surgeries should be performed simultaneously. Therefore, the debate is open to discussion: should the hernia be repaired concomitant to the bariatric procedure? Which bariatric procedure should be performed? Should the hernia be repaired together with the removal of the excess of skin once the patient has lost weight after the bariatric procedure?
There are many arguments in different directions, requiring an extensive analysis of the literature and of the experience by different groups to determine the most appropriate way to proceed.
Special considerations for the treatment of VHs in patients with morbid obesity
There are several factors that have been directly associated with the development of recurrences after conventional open VHR. Among these factors we might identify some related to the hernia, such as the size and location, the number of previous repairs or the presence of non-palpable defects; and others related to local conditions of the surgical wounds, such as the presence of chronic infection or fistulas; and finally some related to the patient, such as age, gender, smoking habit, nutritional status of the patients and morbid obesity.
Regarding obesity, it has been reported that recurrence rate after open hernia repair is 25% in patients with body mass index (BMI) below 25, and rises up to 39% in patients with BMI over 25. However, with laparoscopic repair, this rate decreases significantly, and no differences are observed between obese and non-obese patients. In this sense, Birgisson et al. (2) reported 64 patients who underwent a laparoscopic VH and no significant differences between patients with a BMI less than 29, between 30 and 39 and over 40. Subsequent studies have shown similar results with lower recurrences rates in laparoscopic repair. These results are related to the presence of lower incidence of surgical site infections after laparoscopic repair, making the laparoscopic approach a clear indication for VHRs in obese patients.
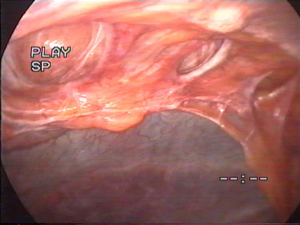
Moreover, we have found that minimally invasive approach allows to identify non-palpable or occult defects on clinical examination, which is another of the most important factors that could influence this decrease of recurrences (Figure 1). In addition, laparoscopic approach also allows to reinforce the entire previous incision around the hernia defect. Previous incision is a weak area where a new hernia can be developed, as it has been demonstrated in several studies. This complete reinforcement of entire previous incision and non-palpable defects can be performed by laparoscopy avoiding an extensive dissection of subcutaneous and musculoaponeurotic tissues reducing the overall wound-related morbidity, which is related to hernia recurrence.
On the other hand, seroma is a very common condition after both open and laparoscopic hernia repair. Risk of seroma infection is lower in the laparoscopic approach, since the access to the cavity with the trocars is far from where this fluid is and remains sterile. While, in open surgery, incision is performed over the defect, in direct contact with the seroma, increasing the possibility of becoming contaminated.
In conclusion, latest meta-analyses have shown that laparoscopic VHR is associated with a lower rate of wound-related morbidity such as infections, hemorrhagic events and the need for mesh removal (3) regardless of patient BMI. These results have led experts to recommend the use of the laparoscopic approach for obese patients in the latest clinical guidelines published (4), since they are one of the groups where the laparoscopic hernia repair presents the most benefits.
However, as in non-obese patients, not all VHs in obese patients are suitable for a minimally invasive repair. It is necessary to establish proper indications of this approach to obtain the best possible results. The need of a concomitant dermolipectomy, trophic skin disorders or a giant defect with loss of domain are some of the cases in which an open approach is recommended even in obese patients. For this reason, an accurate diagnosis is necessary being recommended to perform a CT-scan, since physical examination is difficult in these patients.
Considerations for the treatment of VH in obese patients who is planning a bariatric procedure
A significant percentage of patients undergoing bariatric surgery present a concomitant VH. In most cases it is a primary umbilical hernia, although incisional hernia, even with multiple previous repairs, could also be present. Sometimes, these hernias may be the initial patient’s concern and the reason for medical consultation being referred to a bariatric unit for weight loss prior to abdominal wall reconstruction.
Under these circumstances, several different scenarios are considered, and must be analyzed in order to answer doubts that arise.
Is it safe to perform both surgeries concomitantly by laparoscopy?
Currently, laparoscopic approach is considered the gold standard for bariatric procedures. Under this circumstance, one of the main concerns repairing a VH is the safety of placing a mesh intraabdominally during a bariatric procedure. Most common bariatric procedures, gastric bypass and sleeve gastrectomy, are performed by carrying out gastrointestinal sutures and anastomosis, and are considered as clean-contaminated surgical procedures, and therefore, theoretically there is a risk of potential contamination of the mesh placed inside the abdominal cavity that could be increased in case of a leak or an abscess.
The dilemma of performing both procedures simultaneously had practically no place in the past, when bariatric surgery was performed by open approach. Then the repair of the abdominal wall was mandatory, given the need to access the abdominal cavity through the hernia, considering also that the mesh was placed in the preperitoneal or pre-fascial space, not being in contact with the viscera. In this sense, it was recommended to use meshes prophylactically during the closure of all laparotomies that were performed in obese patients to prevent incisional hernia.
Based on previous considerations, nowadays it could even be recommended to perform an open approach for the bariatric procedure in case of a concomitant VH. This recommendation would even make more sense for supraumbilical incisional hernias, not being recommended in patients with primary supraumbilical or umbilical hernias or incisional hernias located peri or infra-umbilical or in lateral locations. But the current morbidity associated with laparoscopic bariatric surgery, with low incidence of leaks and mortality, technical skills developed by surgeons and the technological advances, make these approaches safer. Currently, there is no data to contraindicate the placement of an intraperitoneal mesh during a bariatric procedure.
In this sense, Sharma et al. (5) published the results of 159 patients who underwent a concomitant bariatric and abdominal wall surgery between 2004 and 2015. Median age of the patients was 53 years, with a mean BMI of 48.2 kg/m2, and 101 females (64%). Comorbidities associated to the patients of this series included: high blood pressure (n=124, 78%), type 2 diabetes (n=103, 65%), hyperlipidemia (n=100, 63%), obstructive sleep apnea (n=98, 62%) and reflux disease (n=54, 34%). Previous VHR was recorded in 41 patients (26%) and 69 patients (44%) had previous abdominal surgery. Ninety-one percent of the interventions were completed laparoscopically (9,144 patients) while 12 (7%) patients were converted to open surgery. Only 3 (2%) patients underwent both procedures by open approach. Different techniques were used to repair the hernia: primary suture in 115 (72%) and mesh repair in 44 patients (28%). Early postoperative complications (<30 days) rate was 10%: superficial wound infection (n=9), intestinal occlusion (n=2), marginal ulcer (n=2), DVT (n=1) and pneumonia (n=1). In terms of recurrences, at 5 years follow up, hernia recurrence rates were 31% in primary repair and 34.8% in mesh repair groups. At 12 months of follow-up, the median BMI and percentage of excess weight loss was 34.2 kg/m2 (IQR: 29.5–40.9) and 59.6% (IQR: 44.9–74.8%), respectively.
According to this study, the existing data in the literature have demonstrated that the bariatric procedure, either a sleeve gastrectomy or a gastric bypass, performed concomitantly with the placement of an intraabdominal mesh to repair a VH (6), is a safe technique that does not increase the morbidity of the procedure and is not associated with a higher rate of recurrences than series of VHRs in obese patients.
When is the best time to repair a VH in an obese patient undergoing bariatric surgery?
But despite the good results published on the repair of VHs concomitantly with the bariatric procedure, there are still doubts whether they should be repaired during the same procedure or it is recommended to defer the hernia repair to avoid the risk of contamination of the mesh. On the other hand, it should be considered to perform the hernia repair once that optimal weight loss has been achieved, since it would be possible to perform the hernia repair in combination with an abdominoplasty in most cases by open approach.
Therefore, the reasons to consider deferring the hernia surgery arises from three considerations: first, due to the possible contamination of the mesh placed intraperitoneally, either due to a dehiscence or a leak, or from a contamination of the abdominal cavity during the anastomosis; second, weight loss frequently leads to an abdominal flap with redundant skin that will require an abdominoplasty and previous repair could make such surgery more difficult; and, third, because there are data that show better results, in terms of recurrences, when a hernia repair is performed after patient’s weight loss.
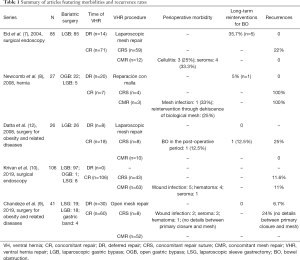
On the other side, those groups who consider performing both surgery at the same time argue that there is a potential risk that the hernia may require an emergency repair because of an acute strangulation after bariatric surgery and during the weight loss period. Eid et al. (7), analyzed 84 patients with VH candidates for bariatric surgery. Seventy-one patients underwent a simultaneous bariatric and hernia repair surgery, while in 14 patients the hernia repair was deferred. This group presented a 37.5% of emergent surgery due to small bowel occlusion during the weight loss period. However, in the series published by Newcomb et al. (8), only 3.7% of the 27 patients with deferred hernia repair after bariatric surgery required emergency surgery. Chandeze et al. (9) analyzed retrospectively 41 bariatric patients with VH; 30 with concomitant surgery (29 with mesh and 1 without a mesh) and 11 who first underwent bariatric surgery and then hernia repair after weight loss. They analyzed the rate of recurrence and observed a lower recurrence in the group in which the hernia repair had been deferred (6.7% vs. 24%), with no differences in postoperative morbidity and a shorter hospital stay lower in group 2 (6.2 vs. 10.7 days).
Krivan et al. (10) recently published a series of 106 patients who underwent a concomitant bariatric and hernia repair surgery (26 incisional and 80 primary hernias). They analyzed the type of approach (open vs. laparoscopic), the type of repair (primary closure vs. mesh repair), defect size (<5, 5–10, >10 cm), type of hernia (primary vs. incisional). Regarding the type of approach, they found a recurrence of 8.47% in concomitant laparoscopic approach vs. a 14.89% in patients with open approach. They observed that 75% of patients who showed a recurrence had defects larger than 5, all of them had a BMI over 45. In respect of morbidity, it could be observed that open incisional hernia repair showed a higher rate of infection and hematoma compared to laparoscopic repair for both incisional and primary hernias, being seroma more frequent after a laparoscopic repair. Authors conclude that concomitant repair (CR) of a VH simultaneously with a bariatric procedure is feasible with a low recurrence rate, showing the laparoscopic approach has lower complication rates than open surgery.
Sait et al. (11) published a systematic review focused on the analysis of the ideal time to perform a VHR in a patient who is going to undergo a bariatric procedure. Conclusions of the review were not consistent since, as we previously observed, some authors recommend CR with the use of a mesh, while others conclude that hernia repair should be performed after bariatric surgery. The studies compiled in this review, with the exception of the one by Datta et al. (12), show that the risk of strangulation of the hernia requiring emergency surgery, appears to increase when the hernia surgery is deferred. The most frequent reason to delay the repair with a synthetic mesh mentioned in this review is the potential risk of contamination, and therefore of infection and removal of the mesh. However, the studies analyzed in this systematic review showed that the risk of infection using a permanent prosthetic mesh may be lower than expected, since three of the five studies did not report mesh related surgical site infections.
But, beside these data, it is evident that we should not generalize and include all patients in the same groups, since not all VHs are similar, existing different locations, lateral or medial and supraumbilical or infraumbilical, being some of them symptomatic while others remain asymptomatic. There are also differences regarding the content; either omentum, small bowel or colon. Different hernia characteristics and locations may change the approach and the recommendation to perform a simultaneous procedure (13,14), even being able to influence on the selection of the bariatric procedure to be performed.
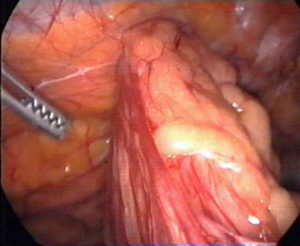
In that sense, some recommendations can be established based on different circumstances (Figure 2). Patients with symptomatic VHs, should undergo a concomitant procedure in order to avoid a repair in a short period of time after surgery. On the contrary, asymptomatic patients could be divided two groups: those with incarcerated omentum (Figure 3), where surgery can be deferred, being recommended not to remove content incarcerated, as it has been demonstrated by Datta et al. (12); or those with bowel incarcerated, where a repair might be necessary before weight loss. In order to be able to follow this algorithm, besides carrying out proper clinical examinations and meticulous analysis of the medical history of the patient, it is recommended to perform a CT scan to determine the characteristics of hernia and its content.

What is the best way to repair a VH in an obese patient who is undergoing a bariatric surgery?
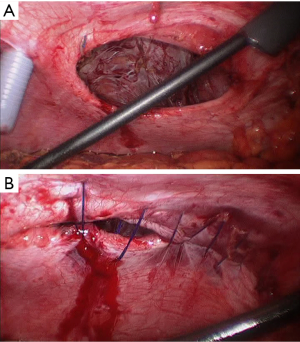
It has been described that it is safe to perform the repair of the VH simultaneously with a bariatric procedure, but there are still doubts about how to technically do it because of the concerns of leaving a mesh intraperitoneally. Laparoscopic primary closure of the defect with transfascial sutures was considered as an alternative (Figure 4A,B), as the mesh is avoided, but a high rate of recurrence has been reported, ranging from 22% to 100%, compared to a 0 to 9% when a mesh is used. Furthermore, the use of this intraperitoneal mesh is not related to an increase of morbidity, being recommended the use of an intraperitoneal mesh in case that a concomitant laparoscopic approach is considered (Figure 5) (7,12,15), being summarize in Table 1. In this sense, Raziel et al. (16) published 54 concomitant laparoscopic VHRs using intraperitoneal meshes during a sleeve gastrectomy or gastric bypass with excellent results.

Full table
In a meta-analysis that included 17,117 patients undergoing sleeve gastrectomy or gastric bypass, it was observed that those patients who underwent simultaneous hernia repair had a slight increase of superficial infections at the surgical site, but without observing an increase in overall morbidity. Regarding the type of concomitant bariatric procedures, no differences were observed between them in terms of complications (17).
Some authors have suggested the use of a biological mesh when a concomitant procedure is performed, since these types of meshes have been recommended in infected, contaminated or potentially contaminated fields. However, although there is no specific data of the use of these prosthetic materials during a bariatric procedure, the use of biological meshes by laparoscopy is associated with an increase in recurrence rates that has even led to cancel previous randomized prospective studies (8,13).
May the presence of a VH influence the type of bariatric procedure to be performed?
The presence of a VH when performing a bariatric procedure might change the original strategy with an obese patient. The first factor to be considered is whether we are dealing with a primary or an incisional hernia. The most common situation in these patients is to find an asymptomatic or minimally symptomatic primary umbilical hernias with omentum, or intraperitoneal fat of the round ligament incarcerated. According to recommendations, it is not indicated to repair these hernias at the time of the bariatric procedure, being very important to avoid reducing the content of the hernia sac to avoid bowel strangulation during the early postoperative period. Also, the presence of this type of hernias should not influence the type of bariatric procedure to be performed based on the protocol of each center. In case of performing a sleeve gastrectomy, trocars should be placed higher than conventional procedure (Figure 6). On the other hand, if a gastric bypass is planned, it is recommended to transect the greater omentum, leaving the area incarcerated on the right side of the patient, allowing an adequate access to the small bowel to perform the anastomosis of the gastric bypass.

In case of an epigastric hernia, different options could be considered depending on the size and the exact location of the hernia; from avoiding the area of the hernia to place the trocars to place the optic trocar through the hernia using and open access, repairing the defect at the end of the procedure with a plug-type mesh, such as the Ventralex® (Bard, Davol, Warwick, RI, USA) or the PVP® (Ethicon, Johnson & Johnson, New Brunswick, NJ, USA).
On the other hand, in the presence of an incisional hernia it is important to consider a series of possible scenarios that may influence the decision on the procedure to be performed. The type of previous surgery is a paramount factor to be considered, since the presence of multiple adhesions could lead us to perform a sleeve gastrectomy instead of a gastric bypass. Infraumbilical incisions with an incisional hernia should not influence the surgical strategy. However, when incisional hernias are related to supraumbilical and supra-infraumbilical incisions, an optic trocar should be placed at the left side of the patient and evaluate the presence of adhesions in order to take the proper decision. Once inside the cavity, a massive adhesiolysis should be avoided. if there is no formal contraindication, a sleeve gastrectomy should be performed, even when originally it was planned to perform a derivative surgery. These procedures should only be performed if the patient does not have massive adhesions when accessing the cavity or there is a contraindication for a sleeve gastrectomy.
Conclusions
The presence of abdominal wall hernias in patients who are candidates for bariatric surgery is a frequent problem. The way we face both pathologies will mark the long-term outcomes. To make a correct decision, multiple factors have to be taken into account; type and location of the hernia and the symptoms it presents. Both, simultaneous surgery and deferring hernia surgery, have their place if a proper selection of patients is performed.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mehmet Mahir Ozmen) for the series “Bariatric and Metabolic Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-20-50). The series “Bariatric and Metabolic Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. SMC reports other from BD Bard, grants and other from Medtronic, other from Ethicon, other from Olympus, other from Storz, other from Stryker, other from Dipro, other from Baxter, from BBraum, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pernar LIM, Pernar CH, Dieffenbach BV, et al. What is the BMI threshold for open ventral hernia repair? Surg Endosc 2017;31:1311-7. [Crossref] [PubMed]
- Birgisson G, Park AE, Mastrangelo MJ Jr, et al. Obesity and laparoscopic repair of ventral hernias. Surg Endosc 2001;15:1419-22. [Crossref] [PubMed]
- Sauerland S, Walgenbach M, Habermalz B, et al. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev 2011;CD007781 [Crossref] [PubMed]
- Cuccurullo D, Piccoli M, Agresta F, et al. Laparoscopic ventral incisional hernia repair: evidence-based guidelines of the first Italian Consensus Conference. Hernia 2013;17:557-66. [Crossref] [PubMed]
- Sharma G, Boules M, Punchai S, et al. Outcomes of concomitant ventral hernia repair performed during bariatric surgery. Surg Endosc 2017;31:1573-82. [Crossref] [PubMed]
- Praveen Raj P, Senthilnathan P, Kumaravel R, et al. Concomitant laparoscopic ventral hernia mesh repair and bariatric surgery: a retrospective study from a tertiary care center. Obes Surg 2012;22:685-9. [Crossref] [PubMed]
- Eid GM, Mattar SG, Hamad G, et al. Repair of ventral hernias in morbidly obese patients undergoing laparoscopic gastric bypass should not be deferred. Surg Endosc 2004;18:207-10. [Crossref] [PubMed]
- Newcomb WL, Polhill JL, Chen AY, et al. Staged hernia repair preceded by gastric bypass for the treatment of morbidly obese patients with complex ventral hernias. Hernia 2008;12:465-9. [Crossref] [PubMed]
- Chandeze MM, Moszkowicz D, Beauchet A, et al. Ventral hernia surgery in morbidly obese patients, immediate or after bariatric surgery preparation: results of a case-matched study. Surg Obes Relat Dis 2019;15:83-8. [Crossref] [PubMed]
- Krivan MS, Giorga A, Barreca M, et al. Concomitant ventral hernia repair and bariatric surgery: a retrospective analysis from a UK-based bariatric center. Surg Endosc 2019;33:705-10. [Crossref] [PubMed]
- Sait MS, Som R, Borg CM, et al. Best evidence topic: Should ventral hernia repair be performed at the same time as bariatric surgery? Ann Med Surg (Lond) 2016;11:21-5. [Crossref] [PubMed]
- Datta T, Eid G, Nahmias N, et al. Management of ventral hernias during laparoscopic gastric bypass. Surg Obes Relat Dis 2008;4:754-57. [Crossref] [PubMed]
- Eid GM, Wikiel KJ, Entabi F, et al. Ventral hernias in morbidly obese patients: a suggested algorithm for operative repair. Obes Surg 2013;23:703-9. [Crossref] [PubMed]
- Rao RS, Gentileschi P, Kini SU. Management of ventral hernias in bariatric surgery. Surg Obes Relat Dis 2011;7:110-6. [Crossref] [PubMed]
- Schuster R, Curet MJ, Alami RS, et al. Concurrent gastric bypass and repair of anterior abdominal wall hernias. Obes Surg 2006;16:1205-8. [Crossref] [PubMed]
- Raziel A, Sakran N, Szold A, et al. Concomitant bariatric and ventral/incisional hernia surgery in morbidly obese patients. Surg Endosc 2014;28:1209-12. [Crossref] [PubMed]
- Spaniolas K, Kasten KR, Mozer AB, et al. Synchronous ventral hernia repair in patients undergoing bariatric surgery. Obes Surg 2015;25:1864-8. [Crossref] [PubMed]
Cite this article as: Morales-Conde S, Licardie E, Socas M, Barranco A, López Bernal F, Alarcón I. Abdominal wall surgery in bariatric patients. Ann Laparosc Endosc Surg 2021;6:33.