
Implementation of IDEAL framework of UK training programme for TaTME
Introduction
Rectal cancer remains one of the most common cancers in the Western world with over 700,000 new cases diagnosed annually and a mortality rate greater than 300,000 (1). Minimal invasive technique has been increasingly used in the management of rectal cancer in last two decades. However, the role of laparoscopy in rectal cancer has been recently questioned as two major randomised controlled trials (RCTs) failed to demonstrate non-inferiority of the laparoscopic approach compared to open (2,3). Conflicting meta-analysis reports have resulted in a lack of consensus of the optimal approach for rectal cancer surgery, resulting in variation throughout daily practice (4,5).
Total mesorectal excision (TME) is considered as gold standard in the treatment of rectal cancer. However, this procedure can be technically difficult especially when tumour is located in the lower third of rectum, in male patient with high body mass index (BMI) and narrow pelvis. Thus, a transanal technique for TME has been developed to conquer the challenges of distal rectal dissections as this offers broader view and possibility of permitting better dissection (6). While initial results were promising, the potential advantages of this approach are yet to be appraised in multicentre RCTs. Despite this, dissemination of transanal total mesorectal excision (TaTME) has speedily unfold across several institutions since the first reported case performed in 2009 (6). The first data analysis from the international TaTME registry has been published, suggesting it an oncologically safe and effective technique with acceptable short-term patient outcomes (7,8).
More recent reports on TaTME specific complications, such as urethral injuries and CO2 embolism, have raised concerns regarding the safety of the procedure (9-12). Lately, early oncological fears have conjointly been raised regarding this technique in Norway and the Netherlands, with high local recurrence rates in a multifocal pattern (13), resulting in the moratorium of this technique in Norway.
It remains unclear whether these issues are related to poor performance of the TaTME technique because of meagrely procedural training or an actual risk factor of the technique itself given the rectotomy created that leaves rectal mucosa exposed to the pelvis and use of high flow insufflators. Until this is fully and scientifically resolved, robust training with a quality assurance mechanism must be in place to ensure patient safety.
A five-stage framework was introduced for scientific evaluation of such innovations: the IDEAL recommendations (14). These recommendations describe five stages of development that occur when new interventional procedures are evaluated and introduced into clinical practice: idea, development, exploration, assessment, and long-term study (14) (http://www.ideal-collaboration.net). In the UK, a national training initiative has been developed as a pilot training programme to aid safe dissemination of this technique (15). The aim of this study was to report on the evolution of the national training initiative for TaTME in the UK, in terms of development, exploration and assessment, using the IDEAL framework.
We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/ales-20-69).
Methods
The study was approved by London Bromley Research Ethics Committee on September 2017 REC reference 15/LO/0499 IRAS project ID 156930.
The evolution of a national pilot training initiative for TaTME is described under the five stages of IDEAL framework (idea, development, exploration, assessment, and long-term study).
Idea of a training programme
The concept of a national training initiative was in response to a member survey of the Association of Coloproctologists of Great Britain and Ireland (ACPGBI) in July 2015 (16). A total of 390 responses were obtained and reported on gaps in education and learning needs for knowledge, technical and non-technical skills and how to meet these challenges in the future (16). This was part of a larger project to develop an educational agenda for the coloproctology society in the UK.
Ninety percent of respondents believed mentorship programmes for TaTME to be very important and 44% estimated 5–10 cases to achieve competency. Analysis of the international TaTME registry also demonstrated a rapid uptake of this novel technique globally and across the UK (17), with many surgeons performing cases without mentorship. Both observations highlighted the need for the concept to develop a structured training programme for this technique in the UK.
Development
Development of consensus on structured training pathway
An international workshop on TaTME was organised in Bristol, UK, on 12 October 2015 (18). The aim of this workshop was to review the results of the above learners’ survey and outline the consensus statements describing the essential elements for structured training programme on TaTME. A bespoke Global Assessment Scale forms were also built during the workshop to be tested on a cadaver model as a formative assessment tool (18). The expert group at the workshop drafted a number of statements for structured training pathway. These were voted on by 78 international experts in the field of TaTME who were nominated by peer recommendations as the pioneers and early implementers of the TaTME technique. A formal Delphi process was carried out to reach a consensus on the various elements of the training pathway (19).
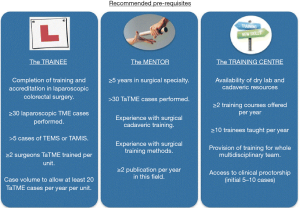
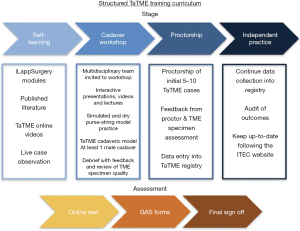
The consensus outcomes and the recommendations summarising the training pathway are outlined in Figures 1,2.
Development of project management and secure funding
A steering group was formed in May 2017 to lead the project, consisting of educational and research leads, representative from ACPGBI, Chair of OCCTOPUS (Oxford Colon Cancer Trust), expert TaTME surgeons from UK, project manager, sponsor and other key stakeholders. The main task of this group was to manage the development and delivery of the training initiative, select the trainers for the programme and monitor the outcomes along with financial performance.
In order to secure funding to support this training initiative, a series of individual discussions and a joint meeting with representatives from an array of healthcare companies was organised in November 2017. The plan for the project was presented and a consortium was formed including four healthcare companies (Medtronic, Applied Medical, Conmed/Lawmed and Stryker) to support this programme. OCCTOPUS, which is a cancer charity and an independent party, was also invited to facilitate and have oversight of this project. The partnership with business industry entailed supporting and facilitating the training that was provided by the expert trainers and while not influencing the educational contents, the training method itself or the outcome data collection and analysis. In order to coordinate the training centrally, an agreement was drawn between the South West Surgical Training Network and OCCTOPUS. The project plan was also presented to the council and the executive board of the ACPGBI, who agreed to endorse the pilot training initiative to ensure quality assurance before wide scale training could be offered.
Selection of the pilot centres
Following the ACPGBI announcement in May 2017, the pilot sites were selected by open and fair method if the centre fulfilled the essential criteria. In order for the sites to be considered, they were required to send an expression of interest with a full application form. The project office received initial interest from over 30 sites. The complete application method required providing details of:
- Colorectal units with two consultant surgeons and associated theatre team;
- Annual caseload for rectal cancer surgery;
- Supporting letter from medical or clinical director affirming the support of the trust during the training period of their staff;
- A business plan or a statement confirming provision of appropriate kit and facility at the trust;
- To ensure the selected surgeons possess the required laparoscopic skills, each consultant surgeon had to submit the unedited version of recent laparoscopic TME for assessment.
The video was assessed objectively by two independent experts using bespoke laparoscopic TME performance tool (L-TMEpt, Figure S1). It was specifically designed for lap TME and its consistency and validity have been approved (20). This form was developed as an extension of LAPCO L-CAT assessment form, previously been utilised as an evidence of competency during the national training for laparoscopic colorectal surgery (21). With the help of the above selection criteria, top five centres that scored highest L-TMEpt score and annual case volume were selected to participate in the national TaTME training initiative.
Selection of proctors
A small group of surgeons with appropriate expertise in TaTME, and a keen interest in teaching, were invited to join the faculty as proctors for this project. They were selected based on their earlier teaching and training credential in previous national laparoscopic colorectal training programme. They were experts who all worked in centre which had high case volume for rectal cancer (over 30), had existing training experience in clinical proctorship and contributed to TaTME registry. They received clear guidance on their role and responsibility within this training initiative and were also invited to join the steering group.
Exploration: clinical training phase
The five selected pilot centres were offered the proctorship programme which was centrally coordinated, funded by educational grants which were made to the healthcare companies. The training programme was multi-modal, including online educational application (App), cadaveric workshop and clinical preceptorship.
Online app
Each consultant was provided free access to the app containing educational modules and videos (http://ilappsurgery.com/app-modules.html) (22). This platform provided them with the knowledge such as case selection, video on steps of operation plus experts’ presentations on tip and tricks and how to avoid pitfalls.
Cadaver workshop
A 2-day cadaveric workshop was organised at the Cushieri Skills Centre (Ninewells Hospital, Dundee). The pilot team (two consultants and their theatre staff who would be working with them) from five selected sites were given the overview of the training initiative by the project lead. Patient selection, theatre setup, operative steps and pitfalls was discussed with the help of series of presentation and debate by the expert faculty. The learners were then able to practice rectal purse string suture on a customized simulator before embarking on a full TaTME on a Thiel preserved human cadaver under the guidance of expert proctors. The bespoke formative Global Assessment tool was also tested in the cadaveric workshop to acquaint both the trainees and trainers with its format and to identify the learning targets during the clinical preceptorship phase.
Clinical preceptorship
Clinical preceptorship was coordinated centrally with the allocation of trainers to the trainees. A team training approach method was implemented whereby the pilot site’s lead surgeon, co surgeon and theatre team received training and guidance on the theatre setup, operative technique and aftercare of the patient. Honorary contract was drawn for each faculty member for a selected pilot site and the process of arranging a preceptored case was then followed. Informed consent was obtained from patients, confirming their participation in the training programme as well as in the study.
Data collection and analysis including assessment tools
On completion of each case, detailed data was entered on the TaTME international registry. This included patient demography, preoperative staging, abdominal and transanal phase of the operation. The primary clinical end point was to obtain high quality TME specimens as defined by Quirke and colleagues for the planes of mesorectal dissection (23). The quality of TME specimen was assessed by means of photographic evidence (anteroposterior and lateral view) and histological examination of the specimen which included distal and circumferential margin status, lymph node yield and lymphovascular invasion. All the above information was entered on the registry including 30 days post-operative complications using the Clavien-Dindo classification.
It was also mandatory to complete the Global Assessment Score (GAS) form designed specifically for TaTME. This was filled independently both by the “trainee” consultant surgeon and “tutor” after each case using a scale of 1 (unable to perform operative step) to 6 (proficient performance) (18).
Assessment
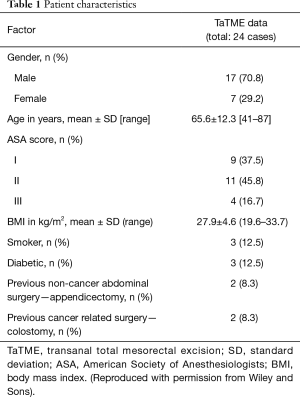
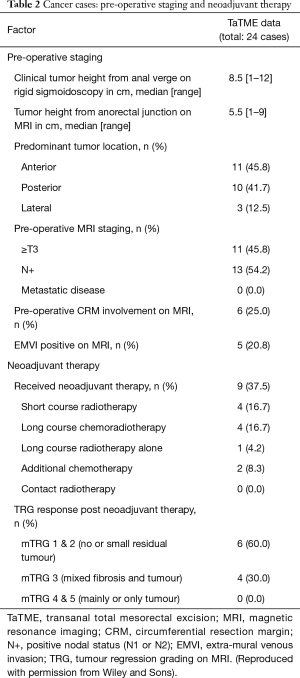
A total of 24 TaTME cases were performed by the trainee consultant surgeon of five pilot sites under mentorship as a part of the national training initiative between November 2017 to October 2018. The patients demographic and tumour characteristic are as detailed in Tables 1,2. Majority of the patients were male (17/24; 70.8%) with a mean age [standard deviation (SD)] 65.6 (12.3) years and BMI of 27.9 (4.6) kg/m2 respectively. On preoperative staging by magnetic resonance imaging (MRI) median tumour distance was 5.5 [1–9] cm and almost fifty percent of tumour was located anteriorly. Neoadjuvant chemotherapy was given in 37.5% of cases (Table 2).
Full table
Full table
Clinical outcomes
Intra-operative results
All 24 cases were performed for rectal cancer of which 20 (83.3%) had low anterior resection and 4 (16.6%) underwent intersphincteric abdomino-perineal excisions (APEs). In view of position of the tumour or patient’s preference given the presence of pre-operative faecal incontinence, three of the above APE were planned procedure. One case was at the start planned as a low anterior resection, however, because of poor blood supply of the left colon, recognised intra-operatively, the procedure was modified to APE. Table 3 outlines additional operative details. All cases were performed using GelPoint Path Transanal Access Platform (Applied Medical, Rancho Santa Margarita, CA, USA) and AirSealTM insufflation system (CONMED, Utica, NY, USA).
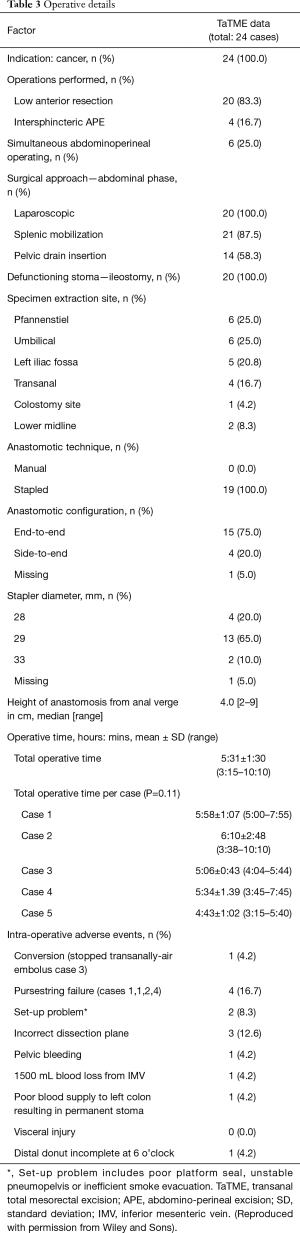
Full table
There was a reduction in median operative time from 331±90 minutes [195–610] in the first case, to 283±62 [195–340] in the final case, however this was not significant.
Reassuringly no visceral injuries occurred intra-operatively throughout any of the 24 cases. Transanal dissection was terminated early in one case because of a gas embolus triggering transient haemodynamic instability. The planned low anterior resection was then completed laparoscopically and the patient was discharged on seventh post-operative day with no additional complications.
There were four purse-string failures which was identified soon after tying the purse-string in place. They were re-inserted under the direction of the mentors without causing any spillage of bowel contents into the operating field.
Post-operative outcomes
Post-operative complications were reported according to Clavien-Dindo classification (I–V). Out of 15 (62.5%) patient who suffered post-operative complications, majority (73.3%) of them were classified as I or II (Table 4). Three (12.5%) patients required emergency surgery within 30 days of the index procedure. The surgical interventions were evacuation and washout of pelvic haematoma, examination under anaesthesia with further stitch placement for anastomosis dehiscence and bilateral leg fasciotomies for compartment syndrome.
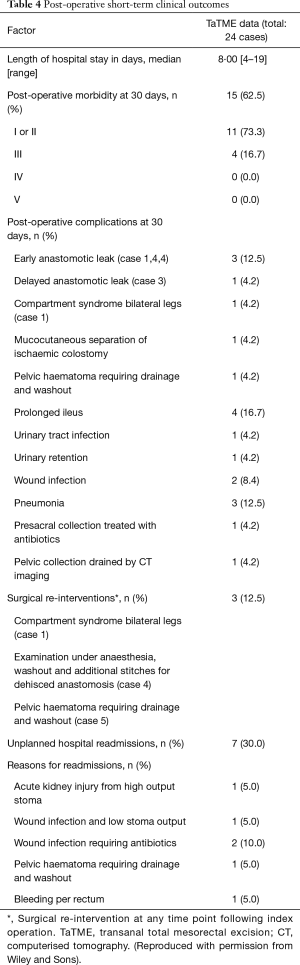
Full table
There was zero 30 days reported mortality.
Late morbidity (diagnosed more than 30 days post-operatively) has been recorded in five cases. They comprise pelvic haematoma following APE which was drained through the perineum, delayed anastomotic leak treated conservatively, parastomal hernia awaiting repair and two cases of chronic sinus (one case following a diagnosed early anastomotic leak).
Histological outcomes
TME specimen was intact in 24 (100%) cases with negative distal resection margin (DRM) in all. However, 1 (4%) had positive circumferential margin (R0 resections 96%). Table 5 describes histological outcomes
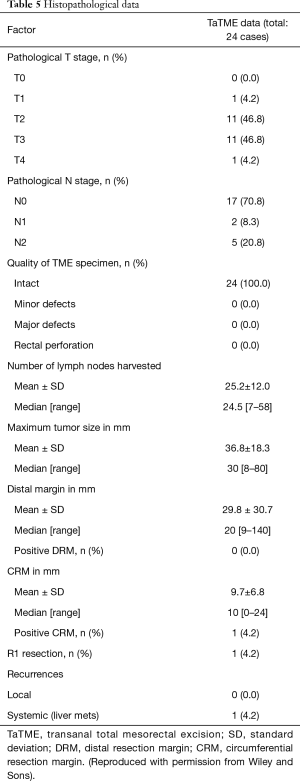
Full table
Educational outcomes
GAS of training
The overall GAS recorded by learners (consultant trainees) and tutors (expert trainers) are shown in Figure S2. Good correlation between trainer and trainee scores was found with an intra-class correlation coefficient of 0.878. All trainees attained competency in overall performance (score 5 or 6) by the time of their final mentored case (Figure S2). A score of at least 4 (performed with minor verbal support) for each operative step was reached by the final mentored case (Figure S3). The posterior and lateral TaTME dissections were found to be most challenging as were given the lowest score on the GAS form stating trainees requiring additional input from the trainers on these areas (Figure S3).
Long-term outcomes
At a median follow-up period of 1 year, (range, 4.2–20.8 months), all patients were alive with no local recurrences but only one case of systemic recurrence with liver metastasis.
Computerised tomography (CT) of the chest, abdomen and pelvis were obtained from only available from 12 patients at 24 months follow up. Three patients developed liver metastases and one developed lung metastasis. There is no evidence of any local or regional recurrences.
Discussion
The IDEAL framework (14) appears to be valuable for the evaluation and reporting of novel techniques, and to aid in the safe disseminating of effective surgical procedures that can be widely adopted. TaTME is an example of a complex novel surgical intervention that has gained a rapid popularity over a very short period of time and not supported by evidence from RCTs or long-term data. It was appropriate to appraise the evolution of the UK training initiative for TaTME using the IDEAL framework (24), given the early reports of technical challenges with visceral injuries and the latest oncological concern about this technique (Table 6).
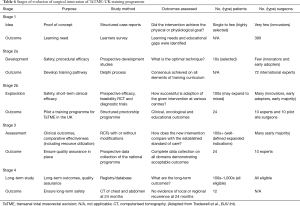
Full table
In this study, IDEAL stage 1 (idea of the training programme) was driven by the rapid change of practice, as surgeons were seeking a better approach/access for low rectal cancer particularly in obese male patients. This overwhelming need coupled with the unsupported rapid uptake of the technique and lack of structured training programme underpinned the concept of the development of training programme.
IDEAL stage 2 (development of the training pathway) followed a formal Delphi process to gain consensus on the essential elements of the training curriculum, including defining the learners, the mentor, the training centre and agreeing on the assessment tools (19). These were implemented in the exploration phase (IDEAL stage 3) of the project to develop and successfully launch a multimodal training programme with online training, cadaveric workshop and clinical preceptorship.
IDEAL stage 4 (assessment) was an integral part of this programme, which demonstrated its clinical and oncological safety. Educational outcomes were also measured objectively with the help of customised validated and reproducible tool.
Long-term outcome (IDEAL stage 5) was captured by radiological imaging and reported no evidence of local or regional recurrence in the available data at 24 months.
IDEAL framework has been reported to monitor safe implementation of innovative surgical techniques (25-27) but there is very little evidence on its application on previous national surgical training programme. There are other training initiatives specifically designed for TaTME in the USA, Australia and Netherlands (9,28,29) which adopted some aspects of quality assurance measures. The UK training model however adopted IDEAL framework as a robust quality assurance across all the stages of the programme from the selection process and up to the follow up surveillance scans.
In a review by Peter McCulloch’s group on the application of the IDEAL framework, the authors found that despite the growing interest and enthusiasm for using IDEAL, the current level of familiarity and usage of the recommendations is low (30). This seems to be mainly due to lack of interpretation of the details of the IDEAL recommendations or how to apply them or omitting important key elements of the framework. In our study, the quality assurance process was developed and prospectively implemented as an integral part of the educational agenda to develop, implement and prospectively evaluate the training programme.
This programme developed and utilised bespoke objective assessment tools which were specifically designed for rectal cancer surgery. This project was the first to report on the application of objective assessment method of technical skills to select the learners. We used a validated tool to ensure competency in laparoscopic TME prior to their selection in TaTME training. The assessment tool (L-TME performance tool) has proven its consistency and validity through a wide evaluation process which involved two RCTs (20). With the aid of application of these robust selection criteria, the project team were able to select five pilot sites that were in the best position to benefit from the training initiative.
Additionally, we developed and utilised GAS forms as formative assessment of surgical skills during the clinical preceptorship phase (18). Such assessments have objectively demonstrated the learning curve of each team and identified the areas that require further training prior to the subsequent case. Implementing these assessment tools is likely to focus and enhance the efficiency of learning which is suggested by the rapid reduction of operative time from case one to five. The GAS forms also objectively demonstrated progression of learner to an independent level with the increasing number of cases.
Furthermore, the programme followed robust prospective clinical assessment criteria with complete data set across a number of domains including clinical, histological, oncological and educational outcomes. These assessment methods reported on a number of technical operative challenges such one gas embolism and one compartment syndrome. Because of the prospective nature of assessment, a full appraisal was carried out for both events and a number of actions were instated to avoid their occurrence which was the case for the rest of the programme. For instance, the insufflation pressure was reduced to as low as feasible enough to maintain adequate rectal wall tension and steep head-down was minimised following the reported incidence of gas embolism. The bilateral compartment syndrome observed in one case (first case) was due to prolonged surgery and mal-positioning of the patient which was corrected on the following cases with no further incidence. This modification was applied across the five pilot sites.
Reassuringly, this programme yielded high quality specimens with no incidence of bowel or tumour perforation and clear distal margins in all specimens and acceptable clear circumferential margins of 96%. One recent article from Norway reported on showing alarming oncological results in terms of high local and multifocal recurrence, resulting in moratorium of this technique in Norway (13), hence it was essential to examine the long-term data. At 1 year (full data) and with the limited data at 2 years (only 50% of cases), there has been no reports of early local or regional recurrence.
This work has a number of limitations. First, despite the comprehensive approach of implementing and reporting on all elements of IDEAL framework, the exploration part targeted to five pilot sites and with only 24 cases. Therefore, one must be careful while drawing any firm conclusions about the outcomes of this phase. The exploration stage however was set up as a pilot initiative to ensure that it was feasible to deliver this multi-modal training to a small number of centres and to carry out robust quality assurance process to demonstrate its safety and feasibleness before wider adoption. Additionally, given the limited available expert trainers for this relatively novel procedure and the financial constraints, it was only possible to provide training to a limited number of centres. Long-term data at 24 months was not complete and we continue to monitor the remaining patients.
The clinical proctorship phase of the programme faced a number of operative challenges, including purse string failure which was noticed in the early stage. This was identified and immediately corrected by the mentor which again demonstrates the importance of preceptorship in the early phase of training. Failure of purse string suture leads to leakage of faecal materials and or cancel cells during the perineal dissection which can potentially increase the local recurrence. This may be a likely mechanism and explanation for the high rates of local recurrences following TaTME reported in Norway leading to the procedure being stopped nationally (13), but further research is required to identify the exact mechanism of this observation, so that a corrective action can be implemented.
Conclusions
A competency based multi-modal training programme for TaTME can be feasible and safe to implement at a national level. Dissemination of a new surgical technique within the confines of a structured surgical innovation IDEAL framework may allow for evidence-based assessment of the technique and may minimize the risk of harm to the patient.
Acknowledgments
We’d like to sincerely thank the Oxford Colon Cancer Trust (Occtopus) for their invaluable oversight and managerial role in this project, as well as the South West Surgical Training Network for centrally co-ordinating the whole initiative. We would also like to thank ACPGBI for believing in and endorsing the initiative and the fantastic team at the Cuschieri Skills Centre, Ninewells Hospital, Dundee, for facilitating the cadaver workshop in a very welcoming and professional environment. Special thanks to our healthcare industry partners (Applied Medical, Conmed/Lawmed, Medtronic and Stryker) who funded and supported the programme throughout its course and allowed it to become reality. Finally, we would like to thank all the trainers and pilot sites surgeons’ who were involved in the exploration phase of this study.
Funding: Special thanks to our healthcare industry partners (Applied Medical, Conmed/Lawmed, Medtronic and Stryker) who funded and supported the programme throughout its course.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Satish Kumar Warrier and Alexander Heriot) for the series “TaTME” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/ales-20-69
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ales-20-69
Peer Review File: Available at http://dx.doi.org/10.21037/ales-20-69
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-20-69). The series “TaTME” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by London Bromley Research Ethics Committee on September 2017 REC reference 15/LO/0499 IRAS project ID 156930.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Stevenson AR, Solomon MJ, Hewett P, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 2015;314:1356-63. [Crossref] [PubMed]
- Fleshman J, Branda M, Sargent DJ, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 2015;314:1346-55. [Crossref] [PubMed]
- Acuna SA, Chesney TR, Ramjist JK, et al. Laparoscopic versus open resection for rectal cancer: a noninferiority meta-analysis of quality of surgical resection outcomes. Ann Surg 2019;269:849-55. [Crossref] [PubMed]
- Martínez-Pérez A, Carra MC, Brunetti F, et al. Pathologic outcomes of laparoscopic vs open mesorectal excision for rectal cancer: a systematic review and meta-analysis. JAMA Surg 2017;152:e165665. [Crossref] [PubMed]
- Sylla P, Rattner DW, Delgado S, et al. NOTES transanal rectal cancer resection using trans-anal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 2010;24:1205-10. [Crossref] [PubMed]
- Hompes R, Arnold S, Warusavitarne J. Towards the safe introduction of transanal total mesorectal excision: the role of a clinical registry. Colorectal Dis 2014;16:498-501. [Crossref] [PubMed]
- Penna M, Hompes R, Arnold S, et al. Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg 2017;266:111-7. [Crossref] [PubMed]
- Atallah SB, DuBose AC, Burke JP, et al. Uptake of transanal total mesorectal excision in North America: initial assessment of a structured training program and the experience of delegate surgeons. Dis Colon Rectum 2017;60:1023-31. [Crossref] [PubMed]
- Dickson EA, Penna M, Cunningham C, et al. International TaTME registry collaborative. carbon dioxide embolism associated with transanal total mesorectal excision surgery: a report from the International Registries. Dis Colon Rectum 2019;62:794-801. [Crossref] [PubMed]
- Harnsberger CR, Alavi K, Davids JS, et al. CO2 embolism can complicate transanal total mesorectal excision. Tech Coloproctol 2018;22:881-5. [Crossref] [PubMed]
- Sylla P, Knol JJ, D'Andrea AP, et al. Urethral injury and other urologic injuries during transanal total mesorectal excision: an international collaborative study. Ann Surg 2019. Epub ahead of print. [Crossref] [PubMed]
- Larsen SG, Pfeffer F, Kørner H, et al. Norwegian moratorium on transanal total mesorectal excision. Br J Surg 2019;106:1120-1. [Crossref] [PubMed]
- McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009;374:1105-12. [Crossref] [PubMed]
- Francis N, Penna M, Carter F, et al. Development and early outcomes of the national training initiative for transanal total mesorectal excision in the UK. Colorectal Dis 2020;22:756-67. [Crossref] [PubMed]
- Francis NK, Curtis NJ, Weegenaar C, et al. Developing a national colorectal educational agenda: a survey of the Association of Coloproctology of Great Britain and Ireland. Colorectal Dis 2018;20:68-73. [Crossref] [PubMed]
- Roodbeen SX, Penna M, Arnold S, et al. A nationwide study on the adoption and short-term outcomes of transanal total mesorectal excision in the UK. Minerva Chir 2019;74:279-88. [Crossref] [PubMed]
- Penna M, Hompes R, Mackenzie H, et al. First international training and assessment consensus workshop on transanal total mesorectal excision (taTME). Tech Coloproctol 2016;20:343-52. [Crossref] [PubMed]
- Francis N, Penna M, Mackenzie H, et al. International TaTME Educational Collaborative Group. Consensus on structured training curriculum for transanal total mesorectal excision (TaTME). Surg Endosc 2017;31:2711-9. [Crossref] [PubMed]
- Curtis NJ, Foster JD, Miskovic D, et al. Association of surgical skill assessment with clinical outcomes in cancer surgery. JAMA Surg 2020;155:590-8. [Crossref] [PubMed]
- Miskovic D, Ni M, Wyles SM, et al. Is competency assessment at the specialist level achievable? A study for the national training programme in laparoscopic colorectal surgery in England. Ann Surg 2013;257:476-82. [Crossref] [PubMed]
- iLappSurgery website (basic modules non-profit). Available online: (Accessed 20 March 2020).http://www.ilappsurgery.com/
- Quirke P, Durdey P, Dixon MF, et al. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumor spread and surgical excision. Lancet 1986;2:996-9. [Crossref] [PubMed]
- Tradewell MB, Albersheim J, Dahm P. Use of the IDEAL framework in the urological literature: where are we in 2018? BJU Int 2019;123:1078-85. [Crossref] [PubMed]
- Blazeby JM, Blencowe NS, Titcomb DR, et al. Demonstration of the IDEAL recommendations for evaluating and reporting surgical innovation in minimally invasive oesophagectomy. Br J Surg 2011;98:544-51. [Crossref] [PubMed]
- Diez del Val I, Loureiro C, McCulloch P. The IDEAL prospective development study format for reporting surgical innovations. An illustrative case study of robotic oesophagectomy. Int J Surg 2015;19:104-11. [Crossref] [PubMed]
- Nikkels C, Vervoort AJMW, Mol BW, et al. IDEAL framework in surgical innovation applied on laparoscopic niche repair. Eur J Obstet Gynecol Reprod Biol 2017;215:247-53. [Crossref] [PubMed]
- Abbott SC, Stevenson ARL, Bell SW, et al. An assessment of an Australasian pathway for the introduction of transanal total mesorectal excision (taTME). Colorectal Dis 2018;20:O1-6. [Crossref] [PubMed]
- Veltcamp Helbach M, van Oostendorp SE, Koedam TWA, et al. Structured training pathway and proctoring; multicenter results of the implementation of transanal total mesorectal excision (TaTME) in the Netherlands. Surg Endosc 2020;34:192-201. [Crossref] [PubMed]
- Khachane A, Philippou Y, Hirst A, et al. Appraising the uptake and use of the IDEAL Framework and Recommendations: a review of the literature. Int J Surg 2018;57:84-90. [Crossref] [PubMed]
Cite this article as: Francis N, Chowdhary M, Penna M, Mortensen N, Hompes R, Carter F. Implementation of IDEAL framework of UK training programme for TaTME. Ann Laparosc Endosc Surg 2021;6:3.


