R-Y gastric bypass and its modifications
It is now clear that sleeve gastrectomy (SG) in a vertical manner is the most preferred weight loss surgical procedure in general, but we can objectively declare that Roux-en-Y gastric bypass (RYGB) is yet one of the most opted procedures in the globe. The announced outcomes of the RYGB studies have a longer history than the relatively contemporary developed methods such as mini-gastric bypass, SG or gastric plication, and the cumulative information on RYGB is more and more than the new techniques (1). Although these recently developed surgical methods have become more popular among the weight loss surgery options, RYGB's former peers such as gastric bands and biliopancreatic diversion lost their supporters over time due to their less efficacy or higher morbidities (1). Some less comprehensive surgical procedures increase the risk of ineffective weight loss and/or failure to cure obesity-related comorbidities and on the other hand, some more complex but more effective procedures cause severe postoperative morbidity that can be hardly treated. RYGB now keep its popularity in most obesity surgery centers and we believe that its popularity is originated from the good balance between its effectiveness and morbidity (1).
As with all bariatric procedures, weight regain can be seen after RYGB. For this reason, besides proximal RYGB, which is accepted as a classic, some modified applications are used in primary or revisional surgery. The objective of this article is making a review that reminds the modified RYGB techniques. Although there are many studies on RYGB modifications in literature, it is seen that there are four types of RYGB operations, proximal, distal, long pouch and banded.
Proximal RYGB
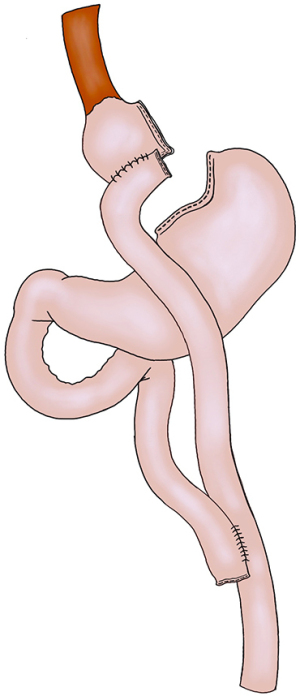
It is not easy to define a standard RYGB technique. However, classical practice involves the Roux-en-Y anastomosis between the proximal small intestine and a limited gastric pouch (Figure 1). It is necessary to mention three separate bowel loops in RYGB. (A) Alimentary loop, (B) Biliopancreatic loop and (C) Common loop (Figure 1). In classical RYGB, while common limb length is not generally measured, alimentary and biliopancreatic leg lengths in the proximal are measured. There are many differences in the literature regarding the length of these loops. The alimentary limb length varies between 50–150 cm, while the biliopancreatic limb length varies between 15–75 cm. For a long time, we have used 50 cm biliopancreatic loop and a 150 cm alimentary loop lengths as standard.
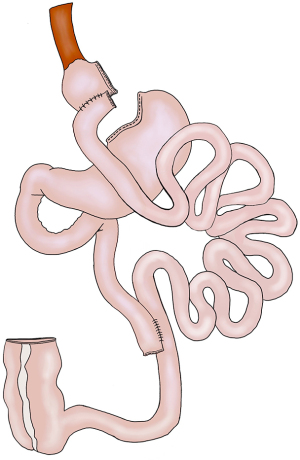
In order to increase metabolic effects such as diabetes, RYGB’s biliopancreatic leg length can be extended. We are still continuing a prospective study investigating the effects of short and long biliopancreatic leg length in diabetic patients. In this modification, the common leg length is not measured. The risk of not measuring the distal remaining gut length may cause an unexpectedly short distal gut length. For this reason, we restrict the length of alimentary limbs to 100 cm instead of 150 cm in patients who have undergone long biliopancreatic limb (150 cm) (Figure 2).
Distal or long limb RYGB
The first long-limb RYGB definition was made by Brolin in 1992. However, in this definition, the biliopancreatic loop was 30 cm and the alimentary loop was 150 cm. In the subsequent definitions, long, very-long and very-very-long limb RYGBs were defined and the biliopancreatic limbs were anastomosed more and more close to the terminal ileum (Figure 2). This modification is usually tried for revisional purposes following weight regain or for super morbid obese people. In 1999, the study of Murr et al., where the biliopancreatic limb was anastomosed to the terminal ileum to 100 cm, was published to report the outcomes of 37 super morbid obese patients (2). With the very-very-long limb RYGB, the average body mass index decreased from 67±3 to 42±2 kg/m2 in 3 years. In the same study, compared to the results of Scapinaro’s biliopancreatic diversion, weight loss rates were similar, but the side effects were less than that of biliopancreatic diversion (2). The same team reported the 4-year results of 257 super obese patients (mean 61±11 kg/m2) in 2006 (3). The mean body mass index of the followed 188 patients decreased to 37±9 kg/m2. They greatly advocate that this more aggressive form of RYGB should not be implemented in patients whose medical surveillance or compliance is questionable (3). We agree with their conclusion that distal type RYGB patients should be closely observed and these procedures should be preserved for the patients who can reach high volume protein consumption. Patients with longer bile and Roux loops provided more type 2 diabetes control, more lipid disorder recovery, and a trend toward rapid excess weight loss (4). It is known that as the common limb prolongs, the risk of liver failure increases (5). Distal RYGB, whose benefit-loss balance is more impaired than proximal RYGB, should be preferred only for revisional surgery or surgery of super-super morbidly obese patients.
Long (extended) pouch RYGB
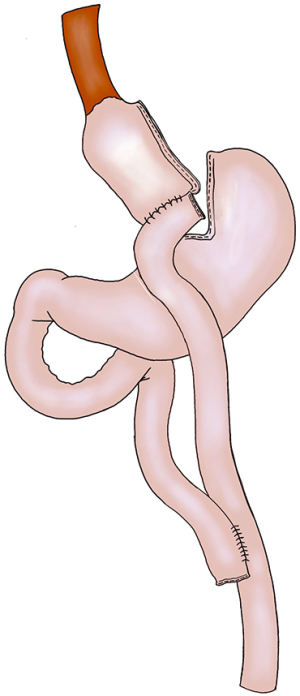
The one anastomosis gastric bypass or mini-gastric bypass is rapidly growing in popularity as a straightforward, effective and safe approach compared to RYGB. It seems to give better results in terms of diabetes control and weight loss in the long term. However, there is still a controversy over the incidence of “biliary reflux” after mini-gastric bypass. Biliary reflux was reported in low incidences (2–4%) but, in case of requirement a revision to RYGB seems mandatory. Ribeiro et al. from Portugal re-formed the one anastomosis gastric bypass by using the same length of biliopancreatic limb with long gastric pouch and by adding a Roux formation with a 100 cm alimentary limb (6). After a four years follow-up, 300 patients lost overall 72% of their excess of weight loss. Long pouch RYGB is an emerging technic and more studies are necessary for its effectiveness (Figure 3).
Banded RYGB
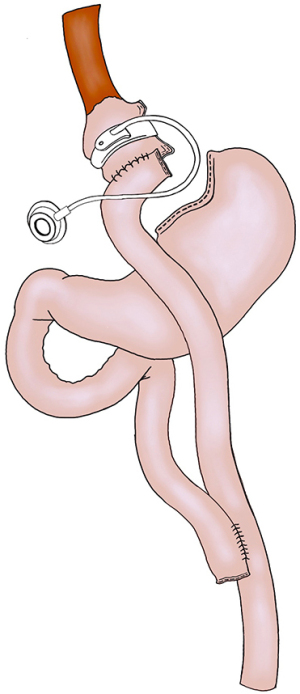
Fobi and co-worker, in 1992, published a RYGB modification involving combination of gastric division and a jejunal loop interposition between the gastric pouch and the bypassed residue; This technique was modified by Fobi et al. by using an adjustable gastric band (Figure 4) (7). In 2014, a comprehensive review was devoted to the mid-term results of banded gastric bypass. The authors evaluated the results of the 8,707 RYGB plus band procedures in 15 publications including the dates between 1990 and 2013. The five-year excess of weight loss was 72.5% (67.5–77.4), and this has not changed significantly for more than 10 years (69.4%). RYGB with an added band is an effective and safe procedure with acceptable rates of early (10.9%) and late (20.0%) morbidities. Banded RYGB has been shown to cause permanent weight loss, perhaps more than that achieved by a standard RYGB. RCTs with longer, comprehensive follow-up rates are needed to fully evaluate the effectiveness and safety of banded RYGB compared to RYGB. Recent evidence suggested that banded RYGB may be an underutilized approach that can effectively serve more patients than it is now.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mehmet Mahir Ozmen) for the series “Bariatric and Metabolic Surgery” published in Annals of Laparoscopic and Endoscopic Surgery.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-2019-bms-11). The series “Bariatric and Metabolic Surgery” was commissioned by the editorial office without any funding or sponsorship. CK serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from Jun 2019 to May 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kayaalp C, Sumer F, Abdullayev A. Laparoscopic Roux-en-Y gastric bypass. Laparosc Endosc Surg Sci 2016;23:110-8. (LESS).
- Murr MM, Balsiger BM, Kennedy FP, et al. Malabsorptive procedures for severe obesity: comparison of pancreaticobiliary bypass and very very long limb Roux-en-Y gastric bypass. J Gastrointest Surg 1999;3:607-12. [Crossref] [PubMed]
- Nelson WK, Fatima J, Houghton SG, et al. The malabsorptive very, very long limb Roux-en-Y gastric bypass for super obesity: results in 257 patients. Surgery 2006;140:517-22. [Crossref] [PubMed]
- Pinheiro JS, Schiavon CA, Pereira PB, et al. Long-long limb Roux-en-Y gastric bypass is more efficacious in treatment of type 2 diabetes and lipid disorders in super-obese patients. Surg Obes Relat Dis 2008;4:521-5; discussion 526-7. [Crossref] [PubMed]
- Ralki M, Cassiman D, Van Dongen J, et al. Liver failure after long-limb gastric bypass. Clin Res Hepatol Gastroenterol 2017;41:e32-7. [Crossref] [PubMed]
- Ribeiro R, Pouwels S, Parmar C, et al. Outcomes of Long Pouch Gastric Bypass (LPGB): 4-Year Experience in Primary and Revision Cases. Obes Surg 2019;29:3665-71. [Crossref] [PubMed]
- Buchwald H, Buchwald JN, McGlennon TW. Systematic review and meta-analysis of medium-term outcomes after banded Roux-en-Y gastric bypass. Obes Surg 2014;24:1536-51. [Crossref] [PubMed]
Cite this article as: Kayaalp C, Sumer F. R-Y gastric bypass and its modifications. Ann Laparosc Endosc Surg 2021;6:51.