
Technical requirements for a safe performance of TAMIS during COVID-19 pandemic: the role of spinal anaesthesia and AirSeal®—a case report
Introduction
Current coronavirus disease 2019 (COVID-19) pandemic, caused by the SARS-CoV-2 virus, is challenging healthcare systems at a global level. All surgical procedures should be performed in highly selective cases (1). It is prudent to postpone non-oncological procedures and prioritize urgent cancer treatment. There should be an optimization of operating room and hospitalization time and complications minimized. The surgical care during the COVID-19 pandemic presents numerous challenges regarding not only patient and community safety, but also the safety of physicians and operating room (OR) staff.
Aerosol generating procedures of respiratory secretions and procedures transmitting droplets can spread the virus. The principles should be to keep droplet spread to a minimum and avoid aerosolization as far as possible (2). In the OR, measures can be taken to reduce the risk of contamination, such as the use of adequate personal protective equipment (PPE). General anaesthesia (GA) not only puts the team at risk but also could induce or exacerbate pulmonary complications in patients with the disease (3). The SARS-CoV-2 virus was identified in the faeces, posing this as a possible route for transmission (4).
The use of minimally invasive surgery during this pandemic should be decided on a case-by-case basis and attention should be paid to limit the leakage of gas from the trocars (1). The AirSeal® System provides active surgical smoke evacuation and filtration for laparoscopic procedures, protecting OR staff.
We present a unique case that describes the role of spinal anaesthesia (SA) combined with AirSeal® device and adequate PPE in reducing the risk of COVID-19 contamination while performing transanal minimally invasive surgery (TAMIS), in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/ales-20-103).
Case presentation
A 59-year-old male patient, with a body mass index (BMI) of 28 kg/m2, was diagnosed with a 3.5 cm T1 rectal adenocarcinoma located 8–10 cm from the anal verge, in the anterior rectal wall, confirmed by magnetic resonance imaging and endoanal ultrasound. His other medical co-morbidities included type II diabetes mellitus, benign prostatic hyperplasia, and gastritis. Blood tests and chest X-ray were normal, thoracoabdominal computed tomography didn’t show any secondary lesions and the electrocardiogram (ECG) revealed an incomplete right bundle branch block. Under these conditions, the patient was considered suitable to undergo the surgical procedure.
The patient was submitted to TAMIS during COVID-19 pandemic due to the risk of oncological progression with delayed treatment. He had no COVID-19 symptoms or risk contacts and the test—viral RNA (ribonucleic acid) detection in a nasopharyngeal swab—was negative. He received standard bowel preparation one day before surgery, thromboprophylaxis and a single dose of 2 g of intravenous cefoxitin and 1 g of intravenous metronidazole for antimicrobial prophylaxis.
In the OR, he was monitored with ECG standard leads, noninvasive monitors for blood pressure, heart rate, arterial oxygen saturation, capnogram and bispectral index (BIS). Spinal block was obtained through a 25 G Quincke® spinal needle introduced in L3–L4 intervertebral space in aseptic conditions, with levobupivacaine 0.5% 2.5 mL (15 mg) and sufentanil (25 mcg). After the spinal block, the patient was placed in the lithotomy position, despite the tumour location (anterior rectal wall). This was done in order to facilitate intubation, if necessary, because of the COVID-19 associated risks. Before surgery, transurethral catheterization was performed, in order to avoid postoperative urinary retention.
Supplemental oxygen with a nasal cannula was given at 2–3 liters per minute. Sensory block level D6 was reached within 5 min after intrathecal injection. Patient’s total comfort was achieved with a target-controlled infusion of propofol to maintain the BIS score at a level of 60–80.
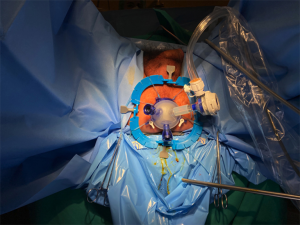
The surgeon started the procedure by doing anal dilation, with appropriate PPE. A Lone Star Retractor® was inserted to optimize the exposure of the anal canal. Next, a Gelpoint path® was placed into the anal muscular cuff (Figure 1) and an AirSeal® system insufflator was used to insufflate continuous CO2 to a pressure of 15 mmHg, establishing the pneumorectum in an airtight platform. Standard laparoscopic instruments (grasper, monopolar electrocautery and a 30-degree laparoscope) were used. The lesion was identified and excised tangentially to the rectal wall, ensuring an adequate oncologic margin of about 1 cm. After the excision of the lesion, the specimen was retained within the rectum and an uninterrupted suture with 2/0 V-lock closed the mucosal defect. After complete pneumorectum evacuation was achieved through the AirSeal® equipment, the Gelpoint Path® was removed and the specimen retrieved. The operation lasted about 45 minutes, having minimum bowel wall flapping and adequate smoke evacuation in this confined environment.
During the procedure, the patient was hemodynamically stable. After surgery, he was shifted to the postanaesthesia care unit for observation and monitoring. There, the patient’s vital signs were stable, and he received 1 g of paracetamol and 2 g of metamizole. Urinary catheter was removed and he had a spontaneous voiding. He got a full recovery of his movement function 4 hours after spinal anaesthesia and was transferred to the surgical ward. He received routine postoperative care and was discharged on postoperative day one without complications. Histologic examination showed tumour free resection margins and, one month after surgery, the patient had no symptoms.
This case report was done in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient.
Discussion
The public health emergency caused by the COVID-19 pandemic has resulted in a reallocation of health resources with a consequent reorganization of the clinical activities. Anaesthesiologists and surgeons are increasingly being faced with patients who need surgery, that are suspected or confirmed cases of COVID-19. Planning for a safe anaesthesia and surgical technique is, consequently, inevitable and extremely important.
The approach may change going towards less invasive procedures to minimize the aerosolized biological fluids (5). Regional anaesthesia is recommended when possible to reduce the risk of COVID-19 transmission, as it avoids aerosol-generating airway procedures (6).
The feasibility and safety of transanal endoscopic microsurgery and TAMIS performed under SA have been demonstrated (7,8). In a study by Lee et al., 25 patients underwent TAMIS for lesions 6–17 cm from the anal verge under SA, without intraoperative complications or postoperative morbidity (8). SA is a less invasive procedure, presents a faster postoperative recovery (7) and is more cost-effective than GA (8). It allows for a quicker recovery and reduced metabolic response to surgical stress, with less postoperative pain, early mobilization, and more oriented and awake patient at the end of the surgery (9), leading to a reduction in hospital length of stay as advocate by the SAGE guidelines (10). For these reasons, SA should be considered the technique of choice for the management of transanal endoscopic surgery, when not contraindicated。 Nowadays, with the COVID-19 pandemic, SA not only has the previously mentioned advantages, but, avoiding an intubation aerosol formation, also protects physicians and other operating room personnel.
On the other hand, one of the challenges using TAMIS is the creation of a stable pneumorectum. Integrated insufflation and access systems (like the AirSeal® system insufflator, together with the Gelpoint path®) can be used to create it and maintain a steady state. They provide high-flow insufflation, continuous pressure sensing, a stable pneumorectum and continuous smoke evacuation during the procedure (11).
Laparoscopic smoke evacuation systems with appropriate filters minimize the aerosol formation and may reduce the risk associated with surgical smoke exposure during this pandemic, although the complete elimination of risk is practically unrealistic (12). This is why adequate PPE is also crucial in the OR (10). The AirSeal® port delivers a valve free access and creates and maintains an invisible barrier, with no air or smoke leak. SARS-CoV-2 virus size ranges from 0.06 to 0.14 µm (12,13). With the AirSeal® system, air and smoke are continuously evacuated through a 0.01 µm ultra-low particulate air (ULPA) filter, effective for SARS-CoV-2 particles (12,13) and better than high efficiency particulate air filter (12). This way, the role of this system is to evacuate the virus from the OR and it can also be used for other procedures besides TAMIS (10).
Although avoiding aerosol formation when combining SA and the AirSeal® system, complete elimination of risk is not well studied, making PPE essential, mainly due to the existence of false negative COVID-19 tests. Also, COVID-19 confirmed patients should be treated in a dedicated OR.
Conclusions
We suggest that TAMIS using proper PPE, Gelpoint path® and AirSeal® under SA can be performed safely during COVID-19 pandemic. If an airtight system can be achieved, all air is evacuated and filtered through the AirSeal®, which can also be used in other laparoscopic procedures. Furthermore, SA reduces the risk of aerosolization during the intubation period and the rapid recovery contributes to a shorter length of stay.
Acknowledgments
The authors would like to thank Dr. António Ribeiro for reviewing our manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/ales-20-103
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-20-103). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This case report was done in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Di Saverio S, Pata F, Gallo G, et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis 2020;22:625-34. [Crossref] [PubMed]
- Australian Society of Anaesthetists. Anaesthesia and caring for patients during the COVID-19 outbreak 2020. Available online: https://asa.org.au/covid-19-updates/
- Chen R, Zhang Y, Huang L, et al. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can J Anaesth 2020;67:655-63. [Crossref] [PubMed]
- Hindson J. COVID-19: faecal-oral transmission?. Nat Rev Gastroenterol Hepatol 2020;17:259. [Crossref] [PubMed]
- Lisi G, Campanelli M, Spoletini D, et al. The possible impact of COVID-19 on colorectal surgery in Italy. Colorectal Dis 2020;22:641-2. [Crossref] [PubMed]
- American Society of Anesthesiologists. Practice Recommendations on Neuraxial Anaesthesia and Peripheral Nerve Blocks during the COVID-19 Pandemic. Available online: https://www.asra.com/page/2905/practice-recommendations-on-neuraxial-anaesthesia-and-peripheral-nerve-blocks-dur
- Allaix ME, Arezzo A, Arolfo S, et al. Transanal endoscopic microsurgery for rectal neoplasms. How I do it. J Gastrointest Surg 2013;17:586-92. [Crossref] [PubMed]
- Lee TG, Lee SJ. Transanal single-port microsurgery for rectal tumors: minimal invasive surgery under spinal anesthesia. Surg Endosc 2014;28:271-80. [Crossref] [PubMed]
- Cortese G, Sales G, Maiolo G, et al. Effectiveness of spinal anesthesia in transanal endoscopic microsurgery: a 3-year experience. Minerva Anestesiol 2018;84:712-9. [PubMed]
- Pryor A. SAGES and EAES recommendations regarding surgical response to COVID-19 crisis. Available online: https://www.sages.org/recommendations-surgical-response-covid-19/
- Bislenghi G, Wolthuis AM, de Buck van Overstraeten A, et al. AirSeal system insufflator to maintain a stable pneumorectum during TAMIS. Tech Coloproctol 2015;19:43-5. [Crossref] [PubMed]
- Resources for smoke & gas evacuation during open, laparoscopic and endoscopic procedures. Available online: https://www.sages.org/resources-smoke-gas-evacuation-during-open-laparoscopic-endoscopic-procedures/
- Cascella M, Rajnik M, Cuomo A, et al. Features, Evaluation, and Treatment of Coronavirus. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2020.
Cite this article as: Amaral MJ, Vaz M, Manso A, Rosete M, Gonçalves N, Serôdio M, Tralhão JG. Technical requirements for a safe performance of TAMIS during COVID-19 pandemic: the role of spinal anaesthesia and AirSeal®—a case report. Ann Laparosc Endosc Surg 2021;6:26.


