Robotic para-aortic lymphadenectomy for isolated colorectal malignancy recurrence: a case report
Highlight box
Key findings
• Robotic para-aortic lymphadenectomy for colorectal metastasis is technically feasible without compromising curative resection.
What is known and what is new?
• Isolated para-aortic lymph node metastasis from colorectal cancer is rare but described, and resection is an accepted treatment
• Historically this was achieved either laparoscopically or via an open approach. We demonstrate the feasibility of robotic resection.
What is the implication, and what should change now?
• Robotic surgery is an effective technique for the management of isolated para-aortic lymph node metastasis. Further research regarding its cost-effectiveness and long-term outcomes should be conducted.
Introduction
Background
Pulmonary and hepatic metastasectomy for colorectal cancer is regularly performed when feasible due to a purposed survival benefit noted in several studies (1). Despite this, there are ongoing investigations on whether this reported benefit in pulmonary metastasectomy is in reality due to an immortal and selection bias (1). While further investigation is warranted, the idea of improved survival following metastasectomy is the main principle behind lymphadenectomy for isolated para-aortic lymph node (PALN) metastasis in colorectal cancer. While this is an established therapy, the staging of isolated PALN metastasis is not consistent across the globe leading to variations in management. There are some guidelines that classify isolated PALN metastasis as regional while others argue it is a distant metastasis or M1 disease, changing management from surgical to medical (2).
Historically, para-aortic lymphadenectomy was performed as an open procedure due to the proximity to vital structures and complexity of resection. With the advent of laparoscopy, and now robotic surgery, some surgeons are considering minimally invasive approaches for this previously open procedure. Para-aortic dissections have been more frequently studied in the gynecologic literature. In one study, they examined laparoscopy vs laparotomy for surgical staging of uterine cancer, including para-aortic lymphadenectomy, and demonstrated adequate oncologic resection, improved quality of life, decreased pain, reduced length of stay, and fewer post operative complications of a minimally invasive approach compared to open (3). It is studies like this that are now paving the way for investigation into a robotic approach for PALN dissection.
Rationale and knowledge gap
It is unknown whether there is a role for robotic surgery in this classically open or laparoscopic procedure. Additionally, there has not been a consensus for the treatment of isolated PALN metastasis in colorectal malignancies and it is unclear whether surgical resection improves outcomes.
Objective
To our knowledge, there is no report of isolated PALN metastasis treated with robotic para-aortic lymphadenectomy without evidence of further recurrence. Our objective in presenting this case is to demonstrate the successful use of robotic surgery in obtaining an adequate oncologic resection while also discussing the role for surgical resection in isolated PALN metastasis for which no consensus of treatment regimen exists. We present this case in accordance with the CARE reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-23-6/rc).
Case presentation
We present a patient who initially presented to our gastroenterology colleagues with 6 months of hematochezia and unintentional weight loss and was referred to our team after a diagnostic colonoscopy diagnosed adenocarcinoma of the rectosigmoid colon. Complete staging workup revealed the tumor to be well proximal to the peritoneal reflection and with notable pericolonic adenopathy. Lesions of the liver and lung were investigated for distant metastasis, but found to be benign by positron emission tomography (PET). Carcinoembryonic antigen was normal. Initial staging was a cT3N1M0 colon adenocarcinoma, and given the resectability of the malignancy, the patient was offered resection. On November 11, 2020, the patient underwent a laparoscopic rectosigmoid resection with tumor directed mesorectal excision and high ligation of the inferior mesenteric artery proximal to the origin of the left colic artery about 1 cm from the aorta, with colorectal anastomosis, which was performed without incident. Final pathology revealed pT4a pN1b cM0 sigmoid adenocarcinoma with 3 of 17 nodes positive. The patient was then seen by medical oncology where they completed adjuvant chemotherapy with 12 cycles of FOLFOX. Following this resection and adjuvant therapy the patient noted resolution of their presenting symptoms of hematochezia and unintended weightloss.
The patient was followed with routine surveillance imaging and approximately 19 months following resection an enlarged lymph node at the aortic bifurcation was incidentally noted on computed tomography (CT). Additional imaging with PET/CT revealed avidity for 18F-fluorodeoxyglucose consistent with a metastatic neoplasm. Endoscopic evaluation did not demonstrate any evidence of local recurrence or synchronous lesions. After a multi-disciplinary tumor board discussion, the patient proceeded with para-aortic lymphadenectomy via robotic approach on July 12, 2022.
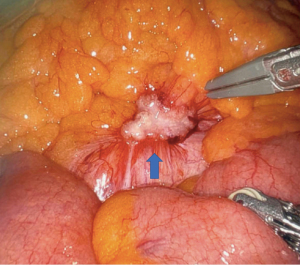
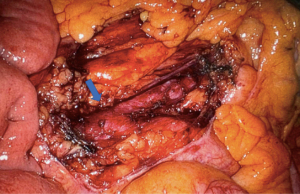
The patient was placed in low lithotomy and a foley catheter was placed. Pneumoperitoneum was established by veress needle without incident and three robotic trocars were placed on the right side of the abdomen (one in the right upper quadrant, one lateral to the umbilicus, and one in the right lower quadrant), so as to have appropriate visualization of the para-aortic retroperitoneum and the site of prior colectomy and anastomosis. Inspection of the abdomen revealed a firm nodule at the base of the colonic mesentery overlying the aorta (Figure 1) consistent in appearance with malignancy. Additional inspection of the peritoneal cavity showed no other suspicious lesions. The peritoneum overlying the para-aortic lesion was then opened with electrocautery, and the mass resected en-block with a 1 cm margin of surrounding mesenteric and retroperitoneal tissue through the use of a robotic bipolar electrocautery device (Figure 2). The remnant of the inferior mesenteric artery was purposely divided at its base by robotic bipolar electrocautery in order to obtain appropriate surgical margins. Indocyanine green angiography was then performed to evaluate perfusion to the remaining colon. This revealed excellent perfusion, with no areas of ischemia (Figure 3). The resected specimen was found to be pathologically consistent with metastatic adenocarcinoma from a colonic primary tumor, with negative resected margins. The patient was discharged home the following day and had an uneventful postoperative recovery.
The patient then followed up with their medical oncologist for additional adjuvant therapy with FOLFIRI and bevacizumab for 6 months. They continue surveillance with their medical oncologist and has not had any further evidence of recurrence.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or relatives after all possible attempts were made.
Discussion
Key findings
Our case provides an example of both the utility of surgical management of isolated para-aortic metastasis following colon resection, as well as the feasibility and effectiveness of a robotic approach to such management.
Strengths and limitations
As with all scientific literature our case report carries both strengths and limitations. The fact that our patient had their initial presentation, resection, recurrence and metastasectomy at one institution with one attending surgeon allows for a more granular and thorough examination of their care from onset through completion. Our case report is obviously limited by the fact that this is a single patient with a relatively rare presentation and disease process.
Comparison with similar researches
Isolated para-aortic recurrence of colorectal malignancy is an exceedingly rare clinical scenario, with a reported incidence around 2% (4). Due to this rarity, there remains to be seen a clear consensus as to whether additional therapy should be medical or surgical in nature. For more common sites of distant metastasis of colon cancer such as the lung and liver, literature has supported the benefit of surgical metastasectomy, and as such it is hypothesized by some that a similar philosophy of resection of isolated para-aortic lymph-node metastasis could also provide benefit to the patient (4).
This hypothesis is supported in some recent retrospective literature, which reports improved overall survival and survival after recurrence in patients with isolated PALN recurrence managed with surgical resection as compared with chemotherapy, although it should be noted the relatively small number of patients in this study (4). Additional retrospective literature investigating colon resection with concurrent resection of PALNs argued that obtaining an R0 resection of primary tumor and nodes had improved survival when compared to management with chemotherapy or R1/R2 resection (5).
While historically PALN dissection was routinely an open procedure with all of the associated morbidity of a midline laparotomy, advancements in laparoscopy and robotic surgery have made a minimally invasive approach technically feasible while still accomplishing adequate resection (6,7). In the gynecology literature there are numerous examples of robotic para-aortic lymph-node dissection, though there remain relatively few reports of this approach for an isolated PALN recurrence of colorectal cancer (6,7). The current data in the gynecologic literature supports an equally successful oncologic resection in both laparoscopic and open approaches for PALN dissection with fewer complications in the laparoscopic group (3). In addition, patients deemed appropriate for metastasectomy indicates oligometastatic disease compared to patient’s not offered metastasectomy which may contribute to differences in survival outcomes (2).
Explanations of findings
This case demonstrates that a robotic approach to para-aortic lymphadenectomy is not only technically feasible but also provides an adequate oncologic resection. To date this patient has not had any further evidence of recurrence. Additionally, this case illuminates several advantages of a robotic approach including the availability of indocyanine green angiography for assessment of colonic perfusion, as well as the well-established advantages in postoperative pain and length of stay seen in minimally invasive surgery as compared to open techniques (6-8).
Implications and actions needed
Given the implied costs of robotic surgery as compared with laparoscopy and open surgery, further investigation is needed regarding the relative cost-effectiveness of robotic lymphadenectomy in this clinical setting. Additionally, further research is needed to determine the benefit of surgical resection for isolated PALN metastasis in colorectal malignancies and the effect this therapy has on overall survival compared to systemic adjuvant chemotherapy.
Conclusions
This case displays an effective treatment option for isolated PALN recurrence of colon malignancy, which is a rare diagnosis with limited literature on appropriate treatment regimens. This case also demonstrates that a robotic approach to this procedure is not only technically feasible but the capability to provide adequate oncologic resection with intra-operative technical advantages including the use of indocyanine green angiography and precise articulated instruments in dissection of the para-aortic nodal basin. Further research is needed to determine if these suspected benefits are cost-effective and truly provide a survival benefit for the patient.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-23-6/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-6/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-6/coif). PCK serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from October 2022 to September 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or relatives after all possible attempts were made.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Treasure T, Macbeth F, Farewell V, et al. The fallacy of large survival gains from lung metastasectomy in colorectal cancer. Lancet 2021;397:97-8. [Crossref] [PubMed]
- Wang RC, Wang JQ, Zhou XY, et al. Survival benefits of para-aortic lymphadenectomy in colorectal cancer with clinically suspected para-aortic lymph node metastasis: a meta-analysis and systematic review. World J Surg Oncol 2023;21:28. [Crossref] [PubMed]
- Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol 2009;27:5331-6. [Crossref] [PubMed]
- Kim YI, Park IJ, Park JH, et al. Management of isolated para-aortic lymph node recurrence after surgery for colorectal cancer. Ann Surg Treat Res 2020;98:130-8. [Crossref] [PubMed]
- Nakai N, Yamaguchi T, Kinugasa Y, et al. Long-term outcomes after resection of para-aortic lymph node metastasis from left-sided colon and rectal cancer. Int J Colorectal Dis 2017;32:999-1007. [Crossref] [PubMed]
- Kim TJ, Yoon G, Lee YY, et al. Robotic high para-aortic lymph node dissection with high port placement using same port for pelvic surgery in gynecologic cancer patients. J Gynecol Oncol 2015;26:222-6. [Crossref] [PubMed]
- Schlappe BA, Leitao MM. Robotic Para-aortic Lymph Node Dissection. In: El-Ghobashy A, Ind T, Persson J, et al. (eds). Textbook of Gynecologic Robotic Surgery. Cham: Springer International Publishing; 2018:131-40.
- Wong JS, Tan GH, Teo MC. Management of para-aortic lymph node metastasis in colorectal patients: A systemic review. Surg Oncol 2016;25:411-8. [Crossref] [PubMed]
Cite this article as: Winder NM, Marcet J, Kuo PC, DeSantis AJ. Robotic para-aortic lymphadenectomy for isolated colorectal malignancy recurrence: a case report. Ann Laparosc Endosc Surg 2023;8:23.