A review of minimally invasive surgery in ulcerative colitis: more than one way to skin a cat
Introduction
While there have been significant advances in biological treatments for ulcerative colitis (UC), there remains a need for operative intervention in approximately 30% of patients. Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the preferred surgery for UC patients with medically refractory disease, refractory bleeding, or dysplasia/cancer. As in most surgical procedures, the move toward minimally invasive surgery (MIS) has improved overall patient outcomes and UC is no exception. Historically patients have undergone laparotomy for total abdominal colectomy (TAC) and IPAA with the frequent need for multistage surgery as well as multiquadrant abdominopelvic surgery presenting a challenge in the adoption of MIS surgery for UC. However, advances in minimally invasive techniques over the last two decades from hand-assist laparoscopy to totally laparoscopic surgery, robotic surgery, and transanal approaches have facilitated the gradual move toward MIS. Clinically, as surgeons, we must continue to adapt and adopt advancing techniques that have been proven to improve patient outcomes. Reviews such as these allow us to adopt these proven techniques and continue to push forward with advancements beyond where our skills currently lie. Here, we will add to the current breadth of knowledge to discuss the various approaches for MIS surgery in UC including the potential advantages and pitfalls of each approach.
Hand-assist laparoscopic surgery
Laparoscopic surgery for UC was first reported in 1992 in two patients undergoing total proctocolectomy with end ileostomy but did not gain popularity early on due to the complex nature of these surgeries and concerns over long operative times (1). Up until the mid-2000s surgery for UC was routinely performed open through a midline laparotomy and the transition to minimally invasive approaches was broached with some trepidation. The concern for fragility of tissues, malnourishment, and immunosuppression in this population were additional concerns that delayed the transition to laparoscopy. In the 2000s, hand-assisted laparoscopic surgery (HALS) gained popularity providing a comfortable transition to laparoscopic surgery. This hybrid approach allowed manual palpation and open access when needed while avoiding a midline laparotomy. TAC was performed through a hand port placed through a Pfannenstiel incision followed by proctectomy, pouch construction, and anastomosis performed open through the Pfannenstiel port (2). Improvements in advanced energy devices using ultrasonic and bipolar energy provided safe vessel sealing and further helped propel MIS for UC. For surgeons starting their laparoscopic careers, HALS TAC had a significantly shorter learning curve than straight laparoscopic TAC (3) and was associated with shorter operative times and fewer conversions to open (4).
Studies showed the safety of HALS for elective IPAA (5-7) and urgent colectomy in fulminant colitis (8,9). Comparative studies showed faster time to bowel function and ambulation, reduced blood loss and shorter hospital stay with HALS vs. open IPAA (10,11). An early randomized trial suggested increased operative time and cost, but no difference in morbidity and postoperative hospital stay with HALS vs. open IPAA (12). However, long-term results of this trial suggested improved body image and cosmesis with HALS IPAA (13). A large case-matched study comparing laparoscopic-assisted (HALS or straight laparoscopic with open pelvic dissection) versus open IPAA found improved pouch function in the laparoscopic assisted group at 1-year postoperatively with decreased number of stools and pad usage but equivalent long-term functional outcomes, quality of life and pouch survival rates (14).
Totally laparoscopic surgery
Despite the many advantages of HALS, the constraints of the bony pelvis prohibited application of HALS in proctectomy, and hence HALS remained a hybrid laparoscopic-open operation for IPAA. With growing experience in MIS, many surgeons transitioned to a totally laparoscopic approach using multiple access ports, with specimen extraction and pouch creation often performed through a Pfannenstiel incision or the ileostomy site. For many surgeons, HALS remained a useful tool and bridge to laparotomy during a difficult dissection. Studies of totally laparoscopic IPAA have shown feasibility and safety (15-18). One feasibility study reported 82 patients undergoing totally laparoscopic IPAA with 11% conversion rate and significant decrease in operative time after the first 40 cases. One-year functional results showed 4.7±1.9 bowel movements daily and 1.0±1.2 nightly bowel movements (18). Compared to open surgery, totally laparoscopic IPAA offers reduced operative blood loss and analgesic drug use, shorter hospital stay and fewer incisional, abdominal and adnexal adhesions (16,19,20). While initial data in the early era of minimally invasive colectomy showed similar clinical outcomes with HALS and totally laparoscopic colectomy (21), more recent data suggests improved outcomes with a totally laparoscopic approach including reduced superficial surgical site infection rates and postoperative ileus (22).
Since totally laparoscopic IPAA includes a laparoscopic proctectomy, impact on sexual function must also be evaluated. A study comparing male and female body image and sexual function after laparoscopic or open IPAA found slightly improved body image in laparoscopic treated women but similar sexual function (23) while another study comparing laparoscopic vs. open rectal dissection during IPAA identified open surgery as a risk factor for erectile dysfunction [odds ratio (OR) =4.16, 95% confidence interval (CI): 1.62–10.65, P=0.003]. In female patients, totally laparoscopic IPAA has also been shown to benefit female fertility and fecundity presumably through decreased pelvic adhesions (24,25).
Expanding on the laparoscopic approach, single-port (SP) IPAA with access through the future ileostomy site in the right lower quadrant has also been reported with successful outcomes (26) but benefits in clinical outcomes over multiport laparoscopy have not been determined.
Laparoscopic IPAA technique
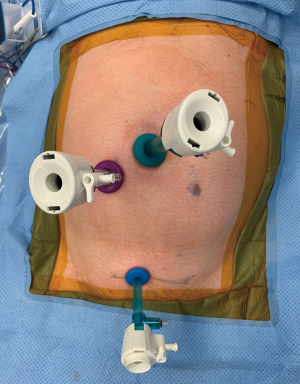
Multiport laparoscopic IPAA is generally performed through 5 port sites with camera port at the umbilicus and extraction through a Pfannenstiel incision. Alternatively, to minimize abdominal incisions, specimen extraction may be performed through future ileostomy site or trans-anally in cases of rectal mucosectomy. In our experience, a 3-port technique (Figure 1) may be used during laparoscopic TAC with a 10-mm periumbilical camera port, a 12-mm working port at the future ileostomy site in the right lower quadrant and a 5-mm suprapubic port. The 10-mm, 30-degree Olympus ENDOEYE (Olympus Medical System Corp, Tokyo, Japan) provides optimal visualization while minimizing instrument clashing through its integrated all-in-one design incorporating the light cable and camera system. This allows the entire colon to be mobilized using a 10-mm LigasureTM blunt tip (Medtronic Inc., Dublin, Ireland) through the 12-mm port at the ileostomy site. A lateral to medial approach working from right to left commences with transection of the rectosigmoid colon where the taenia splay using a 60-mm laparoscopic stapler. The specimen is extracted through the ileostomy site and ileal transection is performed extra-corporeally to prevent blowout of the staple line during extraction through the relatively small ileostomy aperture.
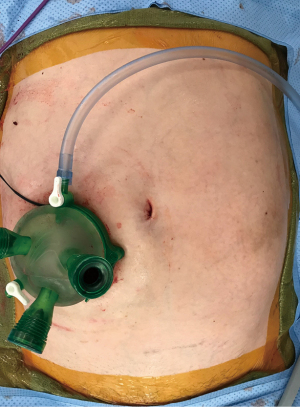
In a staged IPAA, the second stage begins by mobilization of the ileostomy followed by abdominal insufflation and SP laparoscopy using a GelPOINT® Mini Advanced Access Platform (Applied Medical Resources, Rancho Santa Margarita, CA, USA) placed through the ileostomy site (Figure 2). The ileal mesentery is mobilized to the duodenal sweep and pouch length can be assessed intra- and extra-corporeally. Proctectomy is then performed laparoscopically through the GelPOINT® Mini and additional trocars may be placed in the left lower quadrant and umbilicus if needed for visualization and retraction. The superior hemorrhoidal artery is divided close to the bowel to minimize hypogastric nerve injury and dissection is carried in the total mesorectal excision plane posteriorly and close to the rectum laterally and anteriorly to minimize injury to the autonomic nerves and urogenital structures. When rectal mobilization has reached the anorectal ring, a laparoscopic stapler is placed perpendicular to the rectum and appropriate level of transection is confirmed with digital exam or flexible sigmoidoscopy prior to staple firing. This is a crucial step as one of the great limitations to laparoscopic IPAA implicated in pouch failure is an excessively long rectal cuff (27). Another limitation during this portion of laparoscopic IPAA is the need for multiple staple firings to achieve perpendicular rectal transection due to limitations of stapler articulation in the tight space within the bony pelvis. Limiting staple firings to 2 or less is important to minimize anastomotic leak complications (28). In our experience, if this step cannot be completed using 2 or fewer staple firings, a Pfannenstiel incision may facilitate rectal transection using a TATM (Medtronic Inc., Dublin, Ireland) or Echelon CONTOUR stapler (Ethicon Inc., Raritan, NJ, USA). In our practice, pouch construction is performed extracorporeally through the ileostomy site, and double-stapled anastomosis can be achieved under laparoscopic visualization.
Transanal IPAA (taIPAA)
Advances in natural orifice and transanal MIS have yielded considerable interest in transanal proctectomy in the recent decade. Similar to transanal total mesorectal excision (taTME) for rectal cancer, taIPAA for UC is ideal for patients with a narrow and deep pelvis where traditional straight stick laparoscopic instruments may struggle to reach and visualize. Potential advantages of the transanal approach in UC include direct in-line access to the low rectum, consistent rectal transection at the anorectal junction leaving a limited rectal cuff, and omission of multiple staple firings with a single-stapled anastomosis (29,30). Studies comparing taIPAA and transabdominal IPAA have shown safety of taIPAA with short-term (31,32) and long-term outcomes (33,34) comparable to the transabdominal approach. However, in our experience, taIPAA carries a higher rate of anastomotic leak compared with transabdominal IPAA (11% vs. 2%; P=0.03), although this may be attributable to our very low leak rate with conventional transabdominal IPAA (35,36) as our taIPAA leak rates mirror that of other published literature. It is our opinion that transanal IPAA belongs in the toolbox for approaches to IPAA and may be of specific benefit in patients with a particularly narrow and difficult pelvis or in patients with rectal cancer in the setting of UC.
Robotic surgery
The quest for MIS for UC has led many surgeons down the robotic pathway. With improved dexterity, ergonomics, and three-dimensional (3D) visualization, the Da Vinci Surgical System (Intuitive Surgical, Mountain View, Sunnyvale, CA, USA) has been increasingly used for colorectal surgery, and in particular in the pelvis for rectal cancer, prolapse surgery, and IPAA (37-39). Robotic IPAA may be performed totally robotic or hybrid, combining laparoscopic TAC and robotic proctectomy with intracorporeal or extracorporeal creation of the pouch. A recent meta-analysis comparing robotic versus laparoscopic IPAA included 5 non-randomized studies and 3 case series (39). While operating times appeared longer for robotic cases, blood loss was significantly less in 3 out of 4 studies that reported this outcome and hospital stay was shorter in two studies. There was no statistically significant difference in overall complications, hospital readmissions, functional outcomes or quality of life.
SP robotics in the abdomen have only been used in a limited fashion up to this point but may show some promise for minimally invasive procedures in the future. Alternatively, SP Da Vinci transanal proctectomy for cancer has been reported, and may offer an alternative approach for transanal proctectomy in UC (40).
Conclusions
With clear advantages in short-term surgical outcomes including reduced pain, shorter hospital stay, faster return of bowel function, improved cosmesis as well as some potential long-term benefits in bowel function, female fertility, and male sexual function it is clear that MIS for UC is here to stay. Even in the urgent setting with fulminant colitis, laparoscopy is safe and should be preferred over midline laparotomy except in the unstable patient. As we continue to move forward in minimally invasive colorectal surgery we must continue to innovate, especially in those cases that carry the highest morbidity and require the most technical skill. Continued research in single site robotic surgery, taIPAA, and robotics will help drive our patient centered progress forward. It also emphasizes the need for improved training both in domestic programs but also at global UC centers.
In IPAA surgery, surgeon expertise and preference may dictate the minimally invasive approach from laparoscopic, hybrid, transanal, to robotic surgery as studies suggest similar outcomes across the various modalities. Basic principles of quality pouch surgery should always be followed regardless of the minimally invasive approach, including assessment of pouch reach prior to embarking on proctectomy, dissection close to rectum to avoid nerve injury, minimizing cuff length to <2 cm, avoidance of multiple distal rectal staple firings, maneuvers to achieve pouch reach with minimal tension, and construction of a secure anastomosis. Maintaining these principles during minimally invasive IPAA is of utmost importance as construction of a poorly functioning pouch may ultimately destroy patient quality of life, lead to pouch failure, and ultimately permanent ileostomy. Given the relatively young age of patients undergoing IPAA, factors such as fertility, sexual function, and cosmesis remain major factors in their quality of life, satisfaction, and overall wellness and emphasis should be placed on techniques and maneuvers to optimize these outcomes as well. As innovation continues to drive MIS forward, surgeons should prioritize safe pouch surgery by mastering an approach and continuing to incorporate sensical innovation to improve on the long-term outcomes and quality of life of patients having surgery for UC.
Acknowledgments
Special thanks to Dr. Alessandro Fichera (Baylor University Medical Center) for his invitation to participate in this special series on “Minimally Invasive Colorectal Surgery”.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alessandro Fichera) for the series “Minimally Invasive Colorectal Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article has undergone external peer review.
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-7/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-7/coif). The series “Minimally Invasive Colorectal Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration. Informed consent was obtained from the patients for the publication of this article and accompanying images. No IRB was needed as this was a review article about providing the standard of care and images are deidentified.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Peters WR. Laparoscopic total proctocolectomy with creation of ileostomy for ulcerative colitis: report of two cases. J Laparoendosc Surg 1992;2:175-8. [Crossref] [PubMed]
- Agha A, Moser C, Iesalnieks I, et al. Combination of hand-assisted and laparoscopic proctocolectomy (HALP): Technical aspects, learning curve and early postoperative results. Surg Endosc 2008;22:1547-52. [Crossref] [PubMed]
- Ozturk E, Kiran RP, Remzi F, et al. Hand-assisted laparoscopic surgery may be a useful tool for surgeons early in the learning curve performing total abdominal colectomy. Colorectal Dis 2010;12:199-205. [Crossref] [PubMed]
- Boushey RP, Marcello PW, Martel G, et al. Laparoscopic total colectomy: an evolutionary experience. Dis Colon Rectum 2007;50:1512-9. [Crossref] [PubMed]
- Bemelman WA, Ringers J, Meijer DW, et al. Laparoscopic-assisted colectomy with the dexterity pneumo sleeve. Dis Colon Rectum 1996;39:S59-61. [Crossref] [PubMed]
- Shimada N, Ohge H, Yano R, et al. Hand-assisted laparoscopic restorative proctocolectomy for ulcerative colitis. World J Gastrointest Surg 2016;8:578-82. [Crossref] [PubMed]
- Bordeianou L, Hodin R. Total proctocolectomy with ileoanal J-pouch reconstruction utilizing the hand-assisted laparoscopic approach. J Gastrointest Surg 2009;13:2314-20. [Crossref] [PubMed]
- Holubar SD, Larson DW, Dozois EJ, et al. Minimally invasive subtotal colectomy and ileal pouch-anal anastomosis for fulminant ulcerative colitis: a reasonable approach? Dis Colon Rectum 2009;52:187-92. [Crossref] [PubMed]
- Fowkes L, Krishna K, Menon A, et al. Laparoscopic emergency and elective surgery for ulcerative colitis. Colorectal Dis 2008;10:373-8. [Crossref] [PubMed]
- Marcello PW, Milsom JW, Wong SK, et al. Laparoscopic restorative proctocolectomy: case-matched comparative study with open restorative proctocolectomy. Dis Colon Rectum 2000;43:604-8. [Crossref] [PubMed]
- Zhu P, Xing C. Hand-assisted laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis. J Minim Access Surg 2017;13:256-60. [Crossref] [PubMed]
- Maartense S, Dunker MS, Slors JF, et al. Hand-assisted laparoscopic versus open restorative proctocolectomy with ileal pouch anal anastomosis: a randomized trial. Ann Surg 2004;240:984-91; discussion 991-2. [Crossref] [PubMed]
- Polle SW, Dunker MS, Slors JF, et al. Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of a randomized trial. Surg Endosc 2007;21:1301-7. [Crossref] [PubMed]
- Lavryk OA, Stocchi L, Ashburn JH, et al. Case-Matched Comparison of Long-Term Functional and Quality of Life Outcomes Following Laparoscopic Versus Open Ileal Pouch-Anal Anastomosis. World J Surg 2018;42:3746-54. [Crossref] [PubMed]
- Sampietro GM, Colombo F, Frontali A, et al. Totally laparoscopic, multi-stage, restorative proctocolectomy for inflammatory bowel diseases. A prospective study on safety, efficacy and long-term results. Dig Liver Dis 2018;50:1283-91. [Crossref] [PubMed]
- Ouaïssi M, Lefevre JH, Bretagnol F, et al. Laparoscopic 3-step restorative proctocolectomy: comparative study with open approach in 45 patients. Surg Laparosc Endosc Percutan Tech 2008;18:357-62. [Crossref] [PubMed]
- Baek SJ, Dozois EJ, Mathis KL, et al. Safety, feasibility, and short-term outcomes in 588 patients undergoing minimally invasive ileal pouch-anal anastomosis: a single-institution experience. Tech Coloproctol 2016;20:369-74. [Crossref] [PubMed]
- Lefevre JH, Bretagnol F, Ouaïssi M, et al. Total laparoscopic ileal pouch-anal anastomosis: prospective series of 82 patients. Surg Endosc 2009;23:166-73. [Crossref] [PubMed]
- Ozawa H, Nakamura T, Ikeda A, et al. Benefits of a straight laparoscopic restorative proctocolectomy with ileal pouch anal anastomosis for ulcerative colitis: a retrospective case-matched study. Surg Laparosc Endosc Percutan Tech 2012;22:118-21. [Crossref] [PubMed]
- Hull TL, Joyce MR, Geisler DP, et al. Adhesions after laparoscopic and open ileal pouch-anal anastomosis surgery for ulcerative colitis. Br J Surg 2012;99:270-5. [Crossref] [PubMed]
- Marcello PW, Fleshman JW, Milsom JW, et al. Hand-assisted laparoscopic vs. laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum 2008;51:818-26; discussion 826-8. [Crossref] [PubMed]
- Benlice C, Costedio M, Kessler H, et al. Comparison of straight vs hand-assisted laparoscopic colectomy: an assessment from the NSQIP procedure-targeted cohort. Am J Surg 2016;212:406-12. [Crossref] [PubMed]
- Kjaer MD, Laursen SB, Qvist N, et al. Sexual function and body image are similar after laparoscopy-assisted and open ileal pouch-anal anastomosis. World J Surg 2014;38:2460-5. [Crossref] [PubMed]
- Beyer-Berjot L, Maggiori L, Birnbaum D, et al. A total laparoscopic approach reduces the infertility rate after ileal pouch-anal anastomosis: a 2-center study. Ann Surg 2013;258:275-82. [Crossref] [PubMed]
- Bartels SA, D’Hoore A, Cuesta MA, et al. Significantly increased pregnancy rates after laparoscopic restorative proctocolectomy: a cross-sectional study. Ann Surg 2012;256:1045-8. [Crossref] [PubMed]
- Geisler DP, Kirat HT, Remzi FH. Single-port laparoscopic total proctocolectomy with ileal pouch-anal anastomosis: initial operative experience. Surg Endosc 2011;25:2175-8. [Crossref] [PubMed]
- Remzi FH, Aytac E, Ashburn J, et al. Transabdominal Redo Ileal Pouch Surgery for Failed Restorative Proctocolectomy: Lessons Learned Over 500 Patients. Ann Surg 2015;262:675-82. [Crossref] [PubMed]
- Braunschmid T, Hartig N, Baumann L, et al. Influence of multiple stapler firings used for rectal division on colorectal anastomotic leak rate. Surg Endosc 2017;31:5318-26. [Crossref] [PubMed]
- de Buck van Overstraeten A, Wolthuis AM, D'Hoore A. Transanal completion proctectomy after total colectomy and ileal pouch-anal anastomosis for ulcerative colitis: a modified single stapled technique. Colorectal Dis 2016;18:O141-4. [Crossref] [PubMed]
- Zaghiyan K, Warusavitarne J, Spinelli A, et al. Technical variations and feasibility of transanal ileal pouch-anal anastomosis for ulcerative colitis and inflammatory bowel disease unclassified across continents. Tech Coloproctol 2018;22:867-73. [Crossref] [PubMed]
- de Buck van Overstraeten A, Mark-Christensen A, Wasmann KA, et al. Transanal Versus Transabdominal Minimally Invasive (Completion) Proctectomy With Ileal Pouch-anal Anastomosis in Ulcerative Colitis: A Comparative Study. Ann Surg 2017;266:878-83. [Crossref] [PubMed]
- Marker L, Kjær S, Levic-Souzani K, et al. Transanal ileal pouch-anal anastomosis for ulcerative colitis: a single-center comparative study. Tech Coloproctol 2022;26:875-81. [Crossref] [PubMed]
- Capolupo GT, Carannante F, Mascianà G, et al. Transanal proctocolectomy and ileal pouch-anal anastomosis (TaIPAA) for ulcerative colitis: medium term functional outcomes in a single centre. BMC Surg 2021;21:17. [Crossref] [PubMed]
- Bislenghi G, Denolf M, Fieuws S, et al. Functional outcomes of transanal versus transabdominal restorative proctectomy with ileal pouch-anal anastomosis in ulcerative colitis-a monocentric retrospective comparative study. Langenbecks Arch Surg 2022;407:3607-14. [Crossref] [PubMed]
- Truong A, Wood T, Fleshner PR, et al. A Single-Center Experience of Transanal Proctectomy With IPAA for IBD. Dis Colon Rectum 2022;65:1121-8. [Crossref] [PubMed]
- Park L, Truong A, Zaghiyan K, et al. A Single-Center Comparative Study of Open Transabdominal and Laparoscopic Transanal Ileal Pouch-Anal Anastomosis with Total Mesorectal Excision. Has the Bar Been Raised? J Gastrointest Surg 2022;26:1070-6. [Crossref] [PubMed]
- Jayne D, Pigazzi A, Marshall H, et al. Effect of Robotic-Assisted vs Conventional Laparoscopic Surgery on Risk of Conversion to Open Laparotomy Among Patients Undergoing Resection for Rectal Cancer: The ROLARR Randomized Clinical Trial. JAMA 2017;318:1569-80. [Crossref] [PubMed]
- Flynn J, Larach JT, Kong JCH, et al. Robotic versus laparoscopic ventral mesh rectopexy: a systematic review and meta-analysis. Int J Colorectal Dis 2021;36:1621-31. [Crossref] [PubMed]
- Flynn J, Larach JT, Kong JCH, et al. Robotic versus laparoscopic ileal pouch-anal anastomosis (IPAA): a systematic review and meta-analysis. Int J Colorectal Dis 2021;36:1345-56. [Crossref] [PubMed]
- Marks JH, Salem JF, Adams P, et al. SP rTaTME: initial clinical experience with single-port robotic transanal total mesorectal excision (SP rTaTME). Tech Coloproctol 2021;25:721-6. [Crossref] [PubMed]
Cite this article as: Browning C, Zaghiyan K. A review of minimally invasive surgery in ulcerative colitis: more than one way to skin a cat. Ann Laparosc Endosc Surg 2023;8:28.