
Minimally invasive coronary artery bypass grafting: a literature review
Introduction
Background
Since its advent in 1962, coronary artery bypass grafting (CABG) remains the gold standard for coronary artery disease requiring surgical intervention. Limitations of traditional CABG include the need for a median sternotomy and cardiopulmonary bypass, which carry with them significant morbidity in terms of wound complications and coagulopathy. Improvements in medical management and endovascular interventions provide patients with a safe alternative to invasive surgery. As a result, surgical techniques for coronary artery disease have been developed that provide the same therapeutic benefit with less morbidity to the patient.
Rationale and knowledge gap
Advances in minimally invasive techniques in cardiac surgery have centered around limiting the extent of thoracic incisions and operating without the need for cardiopulmonary bypass. The increasing use of robotic platforms has further reduced the morbidity of traditional cardiac surgery. Hybrid approaches that combine endovascular intervention and open repair have also shown promise in improving patient experiences. However, further research is required into whether these approaches provide acceptable outcomes and whether they can be adopted on a broad scale.
Objective
This manuscript discusses the advantages that mini-thoracotomy, robotics, and hybrid platforms can provide the modern cardiac surgeon. It also explores patient selection and cost benefit analysis for minimally invasive CABG. We present this article in accordance with the Narrative Review reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-23-21/rc).
Methods
This study reviews the current literature related to minimally invasive approaches to CABG. A comprehensive literature search was employed using the following search strategy on PubMed: ((“Laparoscopy”[MeSH]) OR (“Robotic Surgical Procedures”[MeSH])) AND ((“Cardiopulmonary Bypass”[MeSH]) OR (“Coronary Artery Bypass”[MeSH]) OR (“Heart Bypass, Left”[MeSH]) OR (“Heart Bypass, Right”[MeSH])). Articles were obtained, screened for applicability, and applied for the chapter review below. This is summarized below in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | January, 2023 |
| Databases and other sources searched | PubMed |
| Search terms used | ((“Laparoscopy”[MeSH]) OR (“Robotic Surgical Procedures”[MeSH])) AND ((“Cardiopulmonary Bypass”[MeSH]) OR (“Coronary Artery Bypass”[MeSH]) OR (“Heart Bypass, Left”[MeSH]) OR (“Heart Bypass, Right”[MeSH])) |
| Timeframe | Up to May, 2023 |
| Inclusion criteria | English studies, all study types considered |
| Selection process | A comprehensive literature review is done and the articles were individually reviewed by two authors |
Results
With the aforementioned strategy, 65 articles were found in the PubMed search. All articles were manually reviewed by two reviewers. Twelve articles were selected based on their relevance to the research topic and the quality of their data. Nine articles were retrospective reviews. Two articles were prospective reviews. One article was an instructional manuscript with a literature review. The Johns Hopkins Textbook of Cardiothoracic Surgery was used for further referencing.
Discussion
Traditional CABG
Traditional CABG through a median sternotomy still remains the most commonly practiced means of surgical bypass. Surgical bypass has still been proven to provide a survival advantage compared to medical therapy in patients with diabetes, critical multivessel coronary disease, and impaired left ventricular function. Hence, minimally invasive modifications are tasked with maintaining this survival benefit while decreasing the size of incisions and improving patient recovery (1).
Mini-thoracotomy: a smaller incision with similar results?
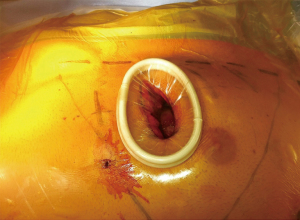
An early advance in minimally invasive CABG was the mini-thoracotomy incision in lieu of the traditional sternotomy (Figure 1). The incision is traditionally carried out through the left fourth intercostal space and allows for the harvesting of the left internal mammary artery (LIMA). The anastomosis can be conducted directly through the mini-thoracotomy incision using conventional surgical instrumentation. This approach can be used with or without the use of cardiopulmonary bypass.
While off-pump surgery does spare patients the hemodynamic and coagulopathic stresses of cardiopulmonary bypass, it may limit the extent of surgery performed. When done off-pump, target anastomosis sites on the beating heart can be held still using suction or pressure stabilizers. These techniques were originally studied by Bonatti and colleague (3).
When mini-thoracotomy was originally introduced, cases were limited to single vessel grafting procedures. Bypass is achieved through peripheral access. The aorta can be traditionally cross-clamped or occluded by an endovascular balloon. Balloon occlusion requires transesophageal echocardiography for safe deployment as well as the absence of aortoiliac or ascending aortic pathology, which is confirmed with preoperative CT angiography of the chest, abdomen, and pelvis (4). Once the balloon is deployed it provides aortic occlusion as well as a means of delivering antegrade cardioplegia. It can also be used to vent the aortic root and measure aortic root pressure. Overall, the mini-thoracotomy incision was one of the first steps toward applying minimally invasive techniques to CABG surgery.
Robotic surgery
The addition of the robot to cardiac surgery has added a new facet to the modern treatment paradigm. Surgeons benefit from improved visualization and better dexterity, and patients avoid the trauma of open surgery. Preoperative cross-sectional imaging allows the surgeon to optimize ergonomics and instrument location. Port placement should account for the space between the pleura and mediastinum to ensure good visualization. As the bony thorax is a fixed space, preoperative measurements can help ascertain the operating space allotted, although they do not account for intraoperative CO2 insufflation and lung deflation (2).
The patient is positioned supine with a shoulder roll under the left chest and the left arm tucked. With the left lung deflated, a camera port is placed in the 4th intercostal space at the anterior axillary line. Next, instrument ports are placed in the 2nd and 6th intercostal spaces at the midclavicular line. Working ports are spaced at least 10 cm apart from the camera port (2) (Figure 2).

The internal mammary artery (IMA) can be harvested using a “no-touch” technique. The parietal pleura is brought down at the second intercostal space. The thoracic fascia is scored medially and laterally allowing for posterior retraction. Then, the LIMA is harvested in either a pedicled or skeletonized fashion until mobilized from the first to the sixth intercostal space. If needed, the right IMA can be accessed by crossing the anterior mediastinum into the right chest (2). Once the appropriate landmarks and vessel targets have been viewed robotically, the mini-thoracotomy is carried out in the optimal location and the anastomosis proceeds through the incision.
The robot can also be used for anastomosis creation, allowing surgeons to forgo a larger open incision. This can be achieved with or without cardiopulmonary bypass, where vessel stabilizers and adjunct anastomosis devices can facilitate surgery on the beating heart. Totally endoscopic coronary artery bypass (TECAB) requires an additional fourth subxiphoid port site for the placement of an endowrist stabilizer (2). Since the mid-2000s, it has been adapted to accommodate multi-vessel disease. Therefore, the robotic platform represents a major step towards implementing a mainstream endoscopic approach to CABG.
Widespread adoption of robotic platforms in the cardiac surgery community has been limited due steep surgeon learning curve, cost, and conflicting efficacy data. Studies demonstrate a triple digit case learning curve required to achieve acceptable outcomes with this procedure, requiring sophisticated simulator modules for surgeon training. Improvement in surgeon skillset is associated with faster harvesting times, operating times, lower rates of open conversion, and better rates of revascularization (5).
Hybrid coronary revascularization (HCR): the best of both worlds?
Surgical coronary revascularization can now be combined with percutaneous coronary intervention (PCI) to provide patients with better outcomes and quicker recovery. HCR includes a surgical bypass, usually with LIMA to the left anterior descending (LAD) branch bypass grafting. This may differ based on patient anatomy and disease. This can be achieved robotically or via a mini thoracotomy. Next, disease in the right coronary and left circumflex systems can be treated with PCI. HCR can be performed in a single or dual-staged manner. While the order may change based on patient needs, surgical bypass is traditionally performed before the PCI. This allows the CABG to be done prior to initiating systemic antiplatelet therapy. It also ensures improved perfusion if higher risk percutaneous measures are needed, such as atherectomy or lithotripsy, that may endanger potential surgical anastomosis sites (6).
Newer generation drug eluting stents (DES) have demonstrated a lower restenosis rate compared to saphenous vein grafts. However, the ability to harvest the IMA bilaterally, and usage of radial or gastroepiploic arteries allows TECAB to improve long-term graft survival and patency rates. Hage and colleagues provide a meta-analysis comparing stand-alone minimally invasive CABG with HCR and demonstrate noninferiority in terms of in-hospital mortality, shock, major adverse cardiac and cerebrovascular event (MACCE), myocardial infarction, and long-term survival. Notably, HCR reduced the need for intensive care unit (ICU) stay, length of hospital stay, and need for blood transfusion. HCR is ideal for the patient with a complex LAD lesion (SYNTAX score >34) and non-complex non-LAD lesions (SYNTAX score less than <22) with no contraindication to dual antiplatelet therapy (DAPT) (7).
Newer data has also shown promise for using a hybrid approach for more than one surgical bypass by harvesting both IMA conduits. Bilateral IMA surgical bypass to perfuse left heart coronary targets has been shown to have an increased survival benefit over single IMA and vein harvest comparisons. In a 2022 single center retrospective study tracking HCR with multivessel TECAB, Nisivaco and colleagues demonstrated an overall 97% graft patency, 98% LIMA-LAD patency, and only a 0.6% mortality rate over an 8-year period. Additionally, complete or near-complete revascularization with PCI adjunct to a residual SYNTAX score less than 8 was associated with a lower mortality and decreased rate of MACCE. With 306 patients having their bypass performed off-pump and on a robotic platform, this is the largest study to date in this patient population. The data demonstrates that HCR maintains the survival benefit of open surgery and also improves outcomes with supplemental PCI (8).
On the other hand, HCR therapy requires post-operative DAPT after stent placement, increasing the theoretical bleeding risk in patients. The body of literature on DAPT in the setting of CABG does report an augmented risk of blood loss, increased transfusions, and a higher rate of re-exploration due to bleeding, and mortality risk. As per the SWEDEHEART registry, administration of clopidogrel and ticagrelor have an intraoperative bleeding risk of 2.7% and 3.7%, respectively, after PCI, which is similar to overall bleeding rates in HCR (9). While HCR combines the best aspects of both open and percutaneous techniques, it should be used selectively.
Patient selection
Appropriate patient selection is vital for good surgical outcomes. Current contraindications to minimally invasive approaches include extensive pleural adhesions, and a history of pleuritis, radiation, or inflammatory thoracic disease. Previous cardiac surgery, limited intercostal space, and significant cardiomegaly also preclude patients from a robotic approach. More medically complex patients with hemodynamic instability are also not candidates. While these constraints are still pertinent, minimally invasive CABG has become available to sicker patients as technology and surgical experience have improved.
Peev and colleagues describe a retrospective review of 100 patients with heart failure with low ejection fraction (left ventricular ejection fraction <40%) who underwent TECAB at a single institution (10). While small, the study boasts a 0% mortality rate and 99% postoperative freedom from angina (10). This is significant since patients with a lower ejection fraction have four times the early postoperative mortality compared to those with a preserved ejection fraction when undergoing open CABG (10).
Minimally invasive approaches have also allowed older patients to undergo coronary artery surgery with less intraoperative risk and better postoperative outcomes. Totally endoscopic surgery allows for shorter ischemia times and acceptable anastomosis times. Off-pump approaches allow for less hemodynamic change during the procedure. This allows for quicker recovery and returns to baseline activity levels. Kitahara and colleagues conducted a retrospective review comparing 28 octogenarians to those under the age of 80 years (11). Postoperative outcomes were similar in terms of hospital length of stay (3.9 vs. 3.5 days). Inpatient mortality was 0% and 78.6% of octogenarians were discharged back home. Thus, TECAB does provide an acceptable risk profile for the elderly (11).
Several studies have looked at how minimally invasive techniques affect female patients. A 6-year retrospective review at the Lankenau Heart Institute conducted a propensity-matched study comparing robot-assisted CABG compared to conventional open off-pump CABG in the female patient. Robotic-assisted surgery resulted in longer operative times, but higher rates of extubation and lower transfusion requirements. Postoperatively, women in the robotic-assisted cohort had shorter stays in the ICU and a shorter hospital stay. As minimally invasive CABG becomes more commonplace, more data will become available for specific demographics of patients (12,13).
Cost
A possible limitation of the growth of minimally invasive CABG in the United States is the burden of financing a robotic program, which includes equipment, maintenance, and personnel. Hospital programs may be deterred from starting a cardiac robotics program when there is no guarantee of the necessary volume to justify the upfront purchase. However, employment of minimally invasive approaches has resulted in a shorter length of stays, shorter ICU times, and lower complication rates, thus being more cost efficient in the long term. Leyvi and colleagues documented a cost analysis comparing robotic CABG to conventional CABG at a single institution with 141 match pair patients. After 30 days, the robotic CABG group demonstrated a lower need for blood transfusion, a shorter length of stay, a shorter ICU stay, and lower rate of composite complications. For the hospital, average costs were nearly equivalent with $18,717.35 for robotic CABG vs. $18,601.00 for conventional CABG. However, in 26 cases of HCR, the average cost was $25,311.10 vs. their conventional CABG matched pairs at $18,966.13. Hence, the cost effectiveness of implementing minimally invasive practices into CABG may present financial obstacles for some institutions (6).
Conclusions
The world of minimally invasive cardiac surgery is undergoing incredible evolution. The strength of these approaches lies in the decreased morbidity of the procedures compared to conventional CABG, as well as a better operative experience for the surgeon. Minimally invasive surgery (MIS) balances the benefit of safe, reliable outcomes with a better perioperative patient experience. As more cases are done, more study should be done regarding the efficiency of minimally invasive CABG from both a time and a cost benefit standpoint, as these are barriers to integration of minimally invasive techniques into standard practice.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Laparoscopic and Endoscopic Surgery for the series “Latest MIS Approaches and Data”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-23-21/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-21/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-21/coif). The series “Latest MIS Approaches and Data” was commissioned by the editorial office without any funding or sponsorship. G.F. served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Laparoscopic and Endoscopic Surgery from April 2023 to March 2025. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yuh DD, Varicella LA, Yang SC, et al. Johns Hopkins Textbook of Cardiothoracic Surgery. 2nd edition. McGraw Hill; 2014.
- Guenther TM, Chen SA, Balkhy HH, et al. Robotic Coronary Artery Bypass Grafting: The Whole 9 Yards. Innovations (Phila) 2020;15:204-10. [Crossref] [PubMed]
- Bonatti J, Wallner S, Crailsheim I, et al. Minimally invasive and robotic coronary artery bypass grafting-a 25-year review. J Thorac Dis 2021;13:1922-44. [Crossref] [PubMed]
- Deshpande SP, Fitzpatrick M, Lehr EJ. Totally endoscopic robotic coronary artery bypass surgery. Curr Opin Anaesthesiol 2014;27:49-56. [Crossref] [PubMed]
- Ravikumar N, George V, Shirke MM, et al. Robotic coronary artery surgery: Outcomes and pitfalls. J Card Surg 2020;35:3108-15. [Crossref] [PubMed]
- Leyvi G, Schechter CB, Sehgal S, et al. Comparison of Index Hospitalization Costs Between Robotic CABG and Conventional CABG: Implications for Hybrid Coronary Revascularization. J Cardiothorac Vasc Anesth 2016;30:12-8. [Crossref] [PubMed]
- Hage A, Giambruno V, Jones P, et al. Hybrid Coronary Revascularization Versus Off-Pump Coronary Artery Bypass Grafting: Comparative Effectiveness Analysis With Long-Term Follow-up. J Am Heart Assoc 2019;8:e014204. [Crossref] [PubMed]
- Nisivaco SM, Kitahara H, Abutaleb AR, et al. Hybrid Coronary Revascularization: Early Outcomes and Midterm Follow-Up in Patients Undergoing Single or Multivessel Robotic TECAB and PCI. Innovations (Phila) 2022;17:513-20. [Crossref] [PubMed]
- Khaliel F, Giambruno V, Chu MWA, et al. Consequences of Hybrid Procedure Addition to Robotic-Assisted Direct Coronary Artery Bypass. Innovations (Phila) 2017;12:192-6. [Crossref] [PubMed]
- Peev MP, Nisivaco S, Torregrossa G, et al. Robotic Off-Pump Totally Endoscopic Coronary Artery Bypass in Patients With Low Ejection Fraction. Innovations (Phila) 2022;17:50-5. [Crossref] [PubMed]
- Kitahara H, McCrorey M, Patel B, et al. Benefit of Robotic Beating-Heart Totally Endoscopic Coronary Artery Bypass in Octogenarians. Innovations (Phila) 2019;14:531-6. [Crossref] [PubMed]
- Tarola CL, Al-Amodi HA, Balasubramanian S, et al. Ultrafast Track Robotic-Assisted Minimally Invasive Coronary Artery Surgical Revascularization. Innovations (Phila) 2017;12:346-50. [Crossref] [PubMed]
- Torregrossa G, Sá MP, Van den Eynde J, et al. Hybrid robotic off-pump versus conventional on-pump and off-pump coronary artery bypass graft surgery in women. J Card Surg 2022;37:895-905. [Crossref] [PubMed]
Cite this article as: Patil R, Zuckerman A, Vu AH, Nha J, Son J, Ferzli G, Vaynblat M. Minimally invasive coronary artery bypass grafting: a literature review. Ann Laparosc Endosc Surg 2024;9:6.


