
Small bowel anastomotic volvulus at reversed loop ileostomy site: a case report
Highlight box
Key findings
• A 57-year-old female with a with a history of laparoscopic proctocolectomy with ileal-pouch anal anastomoses (IPAAs) and loop ileostomy reversal presented with a small bowel anastomotic volvulus at the reversed loop ileostomy site.
What is known and what is new?
• Reversing an ileostomy is a common procedure and is known to have common complications, such as small bowel obstruction, infection, and anastomotic leak.
• This manuscript adds a potential new and rare complication.
What is the implication, and what should change now?
• Based on this case presentation, it is possible for a dilated anastomotic segment to twist about its mesentery and cause a volvulus.
• In patients with small bowel anastomoses who present with bowel obstruction symptoms and signs, it would not be unreasonable to include a small bowel anastomotic volvulus in the list of differentials.
IntroductionOther Section
A small bowel volvulus is a relatively rare condition characterized by the twisting of a loop of intestine and the surrounding mesentery upon itself (1). This condition may stem from several different factors, including predisposing congenital lesions, adhesions from previous surgeries, tumours, or may even occur with no known precipitating etiology. Although an uncommon occurrence, a few cases of pouch volvulus post ileal-pouch anal anastomoses (IPAAs) have been reported in current literature (2-7). In this paper, we present the case of a small bowel anastomotic volvulus at the site of a previously reversed loop ileostomy in a 57-year-old female with a history of laparoscopic proctocolectomy with IPAA and loop ileostomy for ulcerative colitis. Although reversal of an ileostomy has been associated with morbidity and known complications such as small bowel obstruction (SBO), infection, and anastomotic leak, it is rare for a volvulus to occur involving a small bowel anastomosis. The objective of this paper is to describe the details of this case presentation and compare it with current literature. We present this case in accordance with the CARE reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-23-43/rc).
Case presentationOther Section
A 57-year-old female presented to the emergency department with suspected SBO. She had presented with acute abdominal pain and nausea on a background intermittent, progressive, colicky abdominal pain for the past 12 months. She had one previous episode of SBO that had settled conservatively, as well as a past medical history of ulcerative colitis, treated with a laparoscopic proctocolectomy, IPAA and loop ileostomy 15 years prior. The ileostomy was later closed as a side-to-side stapled anastomosis, which was constructed in a side to side “trouser leg” orientation.
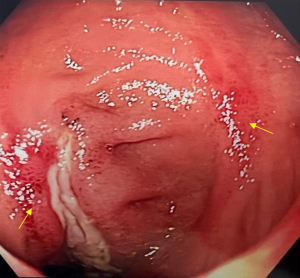
Additionally, routine pouchoscopy for ulcerative colitis surveillance 5 months prior to this presentation demonstrated two areas of non-circumferential ulceration adjacent to a dilated reversed ileostomy site (Figure 1). Biopsies of the ulceration demonstrated no active inflammatory bowel disease. Her IPAA was noted to be normal in appearance.
Her physical examination was consistent with an SBO. Her abdomen appeared distended, with no signs of peritonism. Laboratory results demonstrated an elevated white cell count of 13.6×109/L (4.0–11.0×109/L) and a C-reactive protein of 89 mg/L (<5 mg/L). Computed tomography of the abdomen and pelvis (CTAP) with oral contrast demonstrated findings consistent with a mechanical SBO, concerning for a closed loop obstruction (Figure 2). Urgent transfer to the operating room was arranged.
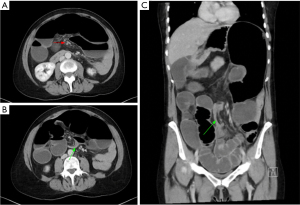
Laparotomy revealed a massive dilation of the previous small bowel anastomosis site (site of closure of ileostomy) to approximately 20 cm. There was significant distension of the proximal small bowel and relative collapse of the distal small bowel, however, no transition point was visible. There were no adhesions in the region contributing to obstruction. The appearances were that the dilated anastomosis was filling with fluid and suspending from the mesentery, allowing the heavy mobile segment to rotate around the mesentery. A flexible colonoscope was passed per rectum to decompress the dilated segment. Two subtle ulcers were visible proximal and distal to the dilated small bowel anastomosis, similar in appearance, to those identified on her previous pouchoscopy. The distal small bowel and the pouch were normal, and no strictures were seen. These findings were suggestive of an intermittent volvulus of the grossly dilated segment. The small bowel mesentery was divided and the previous anastomosis with adjacent dilated small bowel was resected and taken to pathology for analysis (Figure 3). A new side-to-side stapled anastomosis was created.

Subsequently, the patient had prolonged post-operative ileus, but made a full recovery. She continues surveillance in the outpatient setting and remains well. Histopathology of the resected small bowel segment was unremarkable and confirmed the specimen to be a previous small bowel anastomosis with changes consistent with fibrous adhesions and SBO. Importantly, there were no features of inflammatory bowel disease.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
DiscussionOther Section
Diverting ileostomies are created to reduce the rates of anastomotic complications in distal resections (8,9). Reversing an ileostomy is a common procedure, however, it is well documented in the literature to have known complications (10,11). In a retrospective analysis of 132 patients, Poskus et al. found that 24% experienced complications following closure of loop ileostomy and highlighted bowel obstruction as the most common (6.8%), followed by wound infection (3%) and anastomotic leak (2.3%) (11). Similarly, Chow et al. found that bowel obstruction (7.2%) and wound infection (5%) were the most common complications post ileostomy reversal (10). Amongst the known complications stemming from an ileostomy reversal, our case of an intestinal volvulus, involving a chronically dilated anastomosis, has not yet been reported.
An intestinal volvulus generally involves twisting of the bowel around a fixed point, leading to obstruction, oedema, and possibly ischemia or perforation (1). A small bowel volvulus, like in our case, is relatively less common in older adults and usually forms due to adhesions, Meckel’s diverticulum, or a tumour (1,12). Although cases of intestinal volvulus occurring due to an ileostomy reversal have not been reported, there have been few occurrences of “pouch volvulus” following IPAA (2-7). Dionigi et al. noted that among the five patients who suffered a pouch volvulus out of 5,760 who underwent IPAA, all had their surgeries performed via laparoscopy and had minimal adhesions post-surgery (2). They then attributed the lack of adhesions formed post-surgery to be a risk factor in the occurrence of these pouch volvulus (2). Other reported risk factors for pouch volvulus include minimally invasive techniques, female sex, and low body mass index (6). Although our patient has an IPAA, it was not the pouch segment that underwent volvulus, but rather the small bowel anastomosis site from previous loop ileostomy reversal.
It is unclear why a volvulus occurred in our patient, however factors contributing to this may include a chronically dilated anastomosis that had filled with fluid, elongating over time, and subsequently twisting on its mesentery. It is also likely that this was chronic, given her previous surveillance pouchoscopy 5 months earlier demonstrated ulceration adjacent to the anastomoses site and that this was likely due to intermitted volvulus. Supporting this, Le Gal et al. had reported two cases of duodenojejunal anastomosis post pancreas transplant which had undergone volvulus (13). In those patients, both had an anastomosis which had twisted around the mesentery, resulting in a volvulus (13).
Treatment for small bowel volvulus varies depending on each clinical presentation and where in the bowel it occurs. For a small bowel volvulus, this generally involves detorsion of the involved bowel segment and/or resection of the tortuous bowel segment for definitive treatment and prevention of recurrence (1). In our case, the tortuous segment of bowel was decompressed using a flexible colonoscope then resected. Considering the exceptional rarity of this presentation, with no documented occurrences in current literature, the probability of its recurrence was assessed as insignificantly low. Therefore, any modification in our standard practice for anastomosis construction was unwarranted. Consequently, we proceeded to create a new side to side anastomosis of the ileal segments following the resection of the tortuous bowel.
ConclusionsOther Section
A small bowel anastomotic volvulus following reversal of ileostomy is very rare. To our knowledge, this is the first documented case in the literature. Thus, in a patient presenting with obstructive symptoms on a history of ileostomy reversal, it should be included in a list of differential diagnosis.
AcknowledgmentsOther Section
It should be noted that the findings of this paper were presented as a poster at the Annual Cabrini Hospital Research Forum in 2023.
Funding: None.
FootnoteOther Section
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-23-43/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-43/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-43/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Kapadia MR. Volvulus of the Small Bowel and Colon. Clin Colon Rectal Surg 2017;30:40-5. [PubMed]
- Dionigi B, Prien C, Lavryk O, et al. Pouch volvulus-why adhesions are not always the enemy. Colorectal Dis 2022;24:1192-6. [Crossref] [PubMed]
- Jawoosh M, Haffar S, Deepak P, et al. Volvulus of the ileal pouch-anal anastomosis: a meta-narrative systematic review of frequency, diagnosis, and treatment outcomes. Gastroenterol Rep (Oxf) 2019;7:403-10. [Crossref] [PubMed]
- Geers J, Bislenghi G, D’Hoore A, et al. Surgical Management of an Ileal J-Pouch-Anal Anastomosis Volvulus. Dis Colon Rectum 2019;62:1014-9. [Crossref] [PubMed]
- Landisch RM, Knechtges PM, Otterson MF, et al. Pouch Volvulus in Patients Having Undergone Restorative Proctocolectomy for Ulcerative Colitis: A Case Series. Dis Colon Rectum 2018;61:713-8. [Crossref] [PubMed]
- Choughari L, Sohawon S, Noordally SO. Volvulus of an ileoanal J pouch. Int J Colorectal Dis 2010;25:1021-2. [Crossref] [PubMed]
- Chen HLR, Chok AY, Cheng TL, et al. Pouch volvulus after laparoscopic ileal pouch anal anastomosis: the Achilles heel? ANZ J Surg 2022;92:2322-3. [Crossref] [PubMed]
- Hüser N, Michalski CW, Erkan M, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 2008;248:52-60. [Crossref] [PubMed]
- Winslet MC, Barsoum G, Pringle W, et al. Loop ileostomy after ileal pouch-anal anastomosis—is it necessary? Dis Colon Rectum 1991;34:267-70. [Crossref] [PubMed]
- Chow A, Tilney HS, Paraskeva P, et al. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 2009;24:711-23. [Crossref] [PubMed]
- Poskus E, Kildusis E, Smolskas E, et al. Complications after Loop Ileostomy Closure: A Retrospective Analysis of 132 Patients. Viszeralmedizin 2014;30:276-80. [PubMed]
- Spiridakis KG, Sfakianakis EE, Flamourakis ME, et al. Dysfunctional loop ileostomy after low anterior resection for rectal cancer in the presence of Meckel’s diverticulum: a case report. J Med Case Rep 2015;9:192. [Crossref] [PubMed]
- Le Gal A, David A, Loiseau E, et al. Side-to-Side Duodenojejunal Anastomosis Volvulus After Pancreas Transplant: A Case Report. Exp Clin Transplant 2022;21:180-3. [Crossref] [PubMed]
Cite this article as: Feng M, Steen CJ, Bell SW. Small bowel anastomotic volvulus at reversed loop ileostomy site: a case report. Ann Laparosc Endosc Surg 2024;9:10.


