A case report of a 5 mm trocar-site evisceration after transabdominal preperitoneal (TAPP) hernia repair
Highlight box
Key findings
• The presence of hernias in 5 mm trocars is very unusual and can go unnoticed, but we must keep this clinical suspicion in mind. The widespread adoption of minimally invasive surgery makes laparoscopic trocar site hernias a clinically relevant problem.
What is known and what is new?
• The presence of hernias in 5 mm trocars is very unusual.
• To the best of the authors’ knowledge, it is the first obstruction described in a 5 mm trocar after a transabdominal preperitoneal repair. The use of the laparoscopic approach for repair of incarcerated/incisional hernias is increasing, as it is a safe technique with the advantages of being a minimally invasive surgery.
What is the implication, and what should change now?
• The presence of hernias in 5 mm trocars is very unusual and can go unnoticed, but we must keep this clinical suspicion in mind. In cases with high risk and excessive manipulation of the 5 mm trocar, we must try to close the trocars site. This complication, although rare, can appear in the transabdominal approach to inguinal hernias, however, it does not occur with a totally extraperitoneal approach.
Introduction
In the last decades, the minimally invasive approach for surgery, both laparoscopic and robotic, has been adopted and has widely been spread. This development has decreased the incidence of complications related to the abdominal wall, but the morbidity of the abdominal wall has not completely disappeared. Although trocar site herniation is unusual, the widespread adoption of minimally invasive surgery makes laparoscopic trocar site hernias a clinically relevant problem (1).
The first hernia in a laparoscopic trocar was published by Fear in 1968, after a gynecological procedure (2). In 1991, the first case of a hernia in a laparoscopic trocar after a digestive procedure was published by Maio and Ruchman (3).
Incisional hernias in laparoscopic trocar incisions are an infrequent complication, occurring mainly in incisions larger than 10 mm. However, they are usually underdiagnosed and their incidence is likely higher.
The incidence of trocar hernias in large published series ranges between 0.18% and 2.8%; it was 0.74% in a systematic review of 11,699 patients published in 2011 (4). Only a few cases are reported at trocar sites smaller than 10 mm in adult surgery, being even more uncommon in 5 mm incisions with an estimated incidence of 0.0005%. In 2016 a systematic review identified only twenty-seven patients with trocar-site hernias in 5 mm trocars after laparoscopic surgery (5).
Some studies have proposed some risks factors for the appearance of these hernias, such as prolonged surgical time and excessive manipulation of the incisions, which could increase the size of the fascial orifices, such as the use of gauze or hemostatic material through the 5 mm holes as well as the removal and reinsertion of the trocars.
The type of trocar is important; blader trocars have been associated with a greater risk of hernia (6). The place chosen to insert the trocar also is relevant, because the linea alba and the semilunar line are the places with the greatest possibility of herniation, especially at the umbilical level (7). Other factors are obesity, treatment with corticosteroids and patient history of kidney failure or chronic bronchitis. In some studies, female sex and an age over 60 years are proposed as risk factors (5,8).
Another factor that may impact are the use of balloon trocars and the extraction of trocars without completely deflating the balloon, because it could enlarge the defect, increasing the risk of evisceration or eventration in the future.
All of this data lead studies to recommend closing the fascia in trocars larger than 10 mm due to the high risk of hernia. On the other hand, 5 mm ports are not usually closed systematically because it is believed that such iatrogenic fascial defects are not large enough to cause hernias. Based on studies and experience, most surgeons only close defects larger than 10 mm.
Every year, more than 20 million hernias are estimated to be repaired around the world (9). Some studies have shown the advantages of the laparoscopic approach compared to the open Lichtenstein-type approach (10,11); however, the open approach is still considered worldwide as the reference standard for inguinal hernia repair (12).
Transabdominal preperitoneal (TAPP) repair and totally extraperitoneal (TEP) repair are the most frequently used laparoscopic procedures. There are many studies that compare both approaches, and there have been no observed differences in the recurrence and morbidity in either technique (13). The main disadvantage about TAPP approach is the need to access the peritoneal cavity, with the increased risk of bowel injury, future adhesions and trocar site hernias (14). However, the most recent systematic review demonstrated that TEP and TAPP repair were equivalent for median return to sporting activity and showed that postoperative complications between both approaches were comparable (15,16).
Richter hernia is a herniation of the anti-mesenteric portion of the intestine through a fascial defect, the incidence of Richter hernia has been increasing with the growing popularity of minimally invasive surgery and our patient suffered a Richter hernia after a TAPP inguinal hernioplasty. We present this article in accordance with the CARE reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-23-68/rc).
Case presentation
We present a case report of an evisceration through a 5 mm laparoscopic trocar incision after TAPP inguinal hernioplasty.
The patient is a 75-year-old woman, with multiple abdominal surgeries (cesarean section, hysterectomy and double adnexectomy), consulted with our team for a right groin hernia that caused discomfort.
A TAPP hernioplasty is performed as a scheduled surgery, with placement of an umbilical Hasson and two laparoscopic 5 mm balloon trocars in both flanks. We routinely check the abdominal wall after removal of any trocar to verify there is no bleeding or large defects. In this case, the abdominal wall was checked as usually. The patient was discharged the following day, without any complications in the immediate postoperative period.
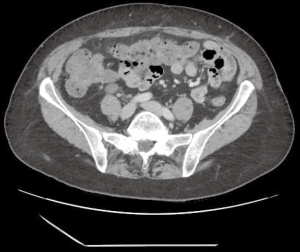
On the third postoperative day, the patient arrived to the emergency room due to diffuse abdominal pain and vomiting during the previous 6 hours. An abdominal X-ray was performed. X-ray findings were suggestive of bowel obstruction including dilated loops of bowel with air-fluid levels. It was initially managed conservatively with placement of a nasogastric tube by emergency doctors. Twenty-four hours after admission to the emergency room, the patient continued to be distended and had no bowel movements, so an abdominal computed tomography (CT) scan was performed that showed a small intestine herniation through a 5 mm laparoscopic trocar incision in the left flank (Figure 1) leading to a mechanical obstruction. The surgical team met the patient after de CT scan. This complication may go unnoticed; therefore, it is important keep this clinical suspicion in mind to diagnose early because time can affect the viability of the involved portion of the bowel.
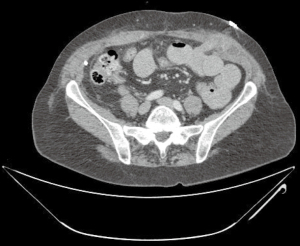
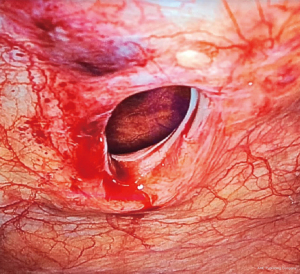
An urgent intervention was performed, using a laparoscopic approach. The herniated ileal loop was identified through the hole of the previous trocar (Figure 2). The incarcerated intestine was reduced, demonstrating its viability without requiring intestinal resection. The abdominal defect measured less than 1 cm (Figure 3), so the defect was closed with barbed suture without using a mesh due to the small size of the hole.
The patient was discharged on the third postoperative day after tolerating a full oral diet and the obstruction was solved. One year later the patient has not presented with a new hernia (Figure 4).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Hernias in laparoscopic trocars are rare, but the standardization of minimally invasive surgery makes them a relevant clinical problem. Hernias in 5 mm trocars are very rare. In a review performed in 2016 only 27 cases were described, although their incidence is possibly higher as they usually are underdiagnosed (5). To the best of the authors’ knowledge, it is the first obstruction described in a 5 mm trocar after a TAPP repair.
Due to its infrequency, the complication of a 5 mm port in the immediate postoperative period, as in our case, may go unnoticed; therefore, we must keep this clinical suspicion in mind. Performing a CT scan in the case of diagnostic doubts may be useful.
There are risk factors for the development of trocar-site hernias on which we cannot act, such as age, comorbidities or obesity. However, we can choose non-cutting, blunt trocars and the smallest possible size, as well as avoid excessive manipulation of the trocars and unnecessary reinsertion of them. There is a consensus for the closure of ports larger than 10 mm whenever possible; however, surgeons do not routinely close 5 mm trocars. In our opinion, we must individualize and in the case of high-risk patients, or when excessive manipulation of the trocars is required, we should try to close these ports to reduce the risk of hernia.
Many groups perform the TAPP repair with a 12 mm trocar to insert a 30-degree laparoscope, and under direct vision an additional 11 mm trocar is placed in the flank to easily insert the mesh. In our experience, we tried to avoid this 11 mm trocar to reduce the trocar site herniation risk, and we placed two 5 mm trocars in each flank.
This complication, although rare, can appear in the transabdominal approach (TAPP) to inguinal hernias; however, it does not happen with an extraperitoneal approach (TEP).
The major advantage of the TEP approach is that an access to the peritoneal cavity is not necessary, so it was considered that TEP may reduce the risks of TAPP caused by a peritoneum entry, so we could have avoided this complication if we had chosen this approach instead of TAPP (17).
The use of a laparoscopic approach for incarcerated primary hernias or incisional hernias is increasing, as it represents a safe and effective technique because of its potential in assess the hernia content, determine the bowel viability and has a decreased incisional infection rate (18-20).
Barbed sutures allow us to close the defect of the abdominal wall, facilitating its laparoscopic closure more easily than with other types of sutures. In our case, due to the small size of the defect, we decided not to place a mesh in the trocar hole during the reintervention, but an alternative could have been to perform a peritoneal flap and place a preperitoneal mesh.
Conclusions
The presence of hernias in 5 mm trocars is very unusual and can go unnoticed, but we must keep this clinical suspicion in mind. This complication can appear in the transabdominal approach to inguinal hernias; however, it does not occur with an extraperitoneal approach (TEP).
The use of the laparoscopic approach for repair of incarcerated/incisional hernias is increasing, as it is a safe technique with the advantages of being a minimally invasive surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-23-68/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-68/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-68/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Swank HA, Mulder IM, la Chapelle CF, et al. Systematic review of trocar-site hernia. Br J Surg 2012;99:315-23. [Crossref] [PubMed]
- Fear RE. Laparoscopy: a valuable aid in gynecologic diagnosis. Obstet Gynecol 1968;31:297-309. [Crossref] [PubMed]
- Maio A, Ruchman RB. CT diagnosis of postlaparoscopic hernia. J Comput Assist Tomogr 1991;15:1054-5. [Crossref] [PubMed]
- Owens M, Barry M, Janjua AZ, et al. A systematic review of laparoscopic port site hernias in gastrointestinal surgery. Surgeon 2011;9:218-24. [Crossref] [PubMed]
- Pereira N, Hutchinson AP, Irani M, et al. 5-millimeter Trocar-site Hernias After Laparoscopy Requiring Surgical Repair. J Minim Invasive Gynecol 2016;23:505-11. [Crossref] [PubMed]
- Azurin DJ, Go LS, Arroyo LR, et al. Trocar site herniation following laparoscopic cholecystectomy and the significance of an incidental preexisting umbilical hernia. Am Surg 1995;61:718-20. [PubMed]
- Tonouchi H, Ohmori Y, Kobayashi M, et al. Trocar site hernia. Arch Surg 2004;139:1248-56. [Crossref] [PubMed]
- Immè A, Cardì F. Incisional hernia at the trocar site in laparoscopic surgery. Chir Ital 2006;58:605-9. [PubMed]
- Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet 2003;362:1561-71. [Crossref] [PubMed]
- Bittner R, Schwarz J. Inguinal hernia repair: current surgical techniques. Langenbecks Arch Surg 2012;397:271-82. [Crossref] [PubMed]
- Memon MA, Cooper NJ, Memon B, et al. Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 2003;90:1479-92. [Crossref] [PubMed]
- Kingsnorth A. Treating inguinal hernias. BMJ 2004;328:59-60. [Crossref] [PubMed]
- Wei FX, Zhang YC, Han W, et al. Transabdominal Preperitoneal (TAPP) Versus Totally Extraperitoneal (TEP) for Laparoscopic Hernia Repair: A Meta-Analysis. Surg Laparosc Endosc Percutan Tech 2015;25:375-83. [Crossref] [PubMed]
- Thalheimer A, Vonlanthen R, Ivanova S, et al. Mind the gap - Small bowel obstruction due to preperitoneal herniation following laparoscopic inguinal hernia repair - A case report. Int J Surg Case Rep 2021;88:106532. [Crossref] [PubMed]
- Kler A, Sekhon N, Antoniou GA, et al. Totally extra-peritoneal repair versus trans-abdominal pre-peritoneal repair for the laparoscopic surgical management of sportsman's hernia: A systematic review and meta-analysis. Surg Endosc 2021;35:5399-413. [Crossref] [PubMed]
- Paajanen H, Montgomery A, Simon T, et al. Systematic review: laparoscopic treatment of long-standing groin pain in athletes. Br J Sports Med 2015;49:814-8. [Crossref] [PubMed]
- Yang S, Zhang G, Jin C, et al. Transabdominal preperitoneal laparoscopic approach for incarcerated inguinal hernia repair: A report of 73 cases. Medicine (Baltimore) 2016;95:e5686. [Crossref] [PubMed]
- Lee SR. Feasibility of Laparoscopic Transabdominal Preperitoneal Hernioplasty for Incarcerated Inguinal Hernia. JSLS 2021;25:e2021.00053.
- Mancini R, Pattaro G, Spaziani E. Laparoscopic trans-abdominal pre-peritoneal (TAPP) surgery for incarcerated inguinal hernia repair. Hernia 2019;23:261-6. [Crossref] [PubMed]
- Memon MA, Fitzgibbons RJ Jr. Laparoscopic Inguinal Hernia Repair: Transabdominal Preperitoneal (TAPP) and Totally Extraperitoneal (TEP) [M]//The SAGES Manual. Berlin, Heidelberg: Springer; 1999:364-78.
Cite this article as: Vilar Tabanera JA, Bru Aparicio M, Quiroga Valcárcel A, Ovejero Merino E, Brabyn P, Gutiérrez Calvo A. A case report of a 5 mm trocar-site evisceration after transabdominal preperitoneal (TAPP) hernia repair. Ann Laparosc Endosc Surg 2024;9:19.