
A narrative review of technical developments for the laparoscopic cholecystectomy
Introduction
The surgical procedure known as cholecystectomy has consistently ranked among the most frequently performed abdominal surgeries since its initial description in 1882. Introduced by the esteemed German surgeon, Professor Müge, in 1985, laparoscopic cholecystectomy (LC) swiftly gained worldwide prominence (1). Presently, LC stands as the definitive “gold standard” in the surgical management of gallstone disease. This procedure has universally supplanted the traditional open cholecystectomy, primarily due to its confluence with the advantages characteristic of laparoscopic surgical approaches. These advantages encompass reduced postoperative pain, enhanced aesthetic outcomes, shorter hospitalization durations, reduced work absenteeism, and the absence of necessity for specialized techniques or exceedingly advanced instrumentation (2). To this end one of the most common interventions performed worldwide in general surgery clinics. Even though the risk of dangerous complications such as duct injury is slightly higher than with traditional cholecystectomy (0.2–0.3% of cases) LC (0.4–1.5% of cases) remains the gold standard for patients with gallstone disease (3). In current literature has reported all types of bile duct injuries (BDIs) occurred in 0.4 and 0.8 percent of elective and emergency settings, respectively (3). BDIs can cause serious morbidity, loss of quality of life, and mortality of up to 3.5% for patients (3).
In its nascent stages, LC involved the identification, ligation, and transection of the cystic artery and duct, culminating in the separation of the gallbladder from the liver bed—referred to as the infundibular technique. Simultaneously, dissection until the choledocho-cystic junction was uncovered were employed or antegrade dissection as alternative methodologies. However, due to initial inexperience in implementing this novel technique and its insufficiency in ensuring the safety of LC, there was a notable surge in the incidence of BDIs compared to open surgical interventions. Strasberg et al. have demonstrated that approximately 80% of iatrogenic injuries in LC are associated with the use of the infundibular technique (4). Furthermore, major vascular injuries, which may necessitate liver transplantation, are more prevalent in cases involving the antegrade technique (5). Consequently, the globally recognized concept of the “Critical View of Safety” as articulated by Strasberg, has gained acceptance and serves as a foundational framework, albeit with certain adaptations introduced and adopted by surgeons (6,7).
Following the widespread embrace of safe surgical principles in LC, surgeons have endeavored to devise modifications aimed at enhancing postoperative outcomes and aesthetic results. In pursuit of this objective, the LC technique has undergone a multitude of refinements and variations over time, yielding a diverse array of more than 50 distinct LC techniques documented in the medical literature (8). Most of these innovations are designed to reduce the dimensions and quantity of ports employed in comparison to those traditionally employed in the standard LC procedure.
Background
Standard LC
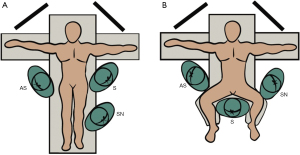
LC is typically performed under general anesthesia. The patient is positioned in the supine orientation on the operating table. In the American approach, the surgeon and camera operator position themselves to the patient’s left, while the assistant stands to the right. Conversely, the French style entails the patient’s supine placement with abducted legs, with the surgeon positioned between the legs, the camera operator on the left, and the assistant on the right (Figure 1). After establishing pneumoperitoneum and inserting trocars, the patient is repositioned into the reverse Trendelenburg position, with the left side lowered (9).
The first entry into the abdominal cavity is typically made through the umbilical region using either an open (Hasson) or closed (Veress needle) technique. Alternatively, a visual trocar may assist in the initial entry. Literature debates the advantages and drawbacks of these methods, with individual surgeon preference often dictating the choice. In the absence of specific indications, the umbilicus the preferred entry points due to its relatively thin subcutaneous tissue, facilitating safe and straightforward access. Generally, a 10-mm telescope is introduced through the umbilical trocar. Subsequently, the abdominal cavity is explored, assessing for any anomalies such as masses, inflammation, or peritoneal adhesions. Additional entry points are chosen with meticulous consideration to avoid any harm. The assistant’s 5-mm trocar is typically positioned at the junction of the anterior axillary line and a line extending toward the left lateral aspect of the umbilicus. Another trocar, measuring either 5 or 10 mm, is placed in the high epigastric/subxiphoid region to accommodate the surgeon’s right-hand instruments, positioned just to the right of the falciform ligament. The size of this trocar is contingent upon the clip applicator’s dimensions. Latest 5 mm trocar for the surgeon’s left-hand instruments is placed along the right mid-clavicular line, approximately 2–3 cm below the costal arch (Figure 2). Careful planning is essential to avoid potential interference with the epigastric artery and vein, which may result in bleeding or hematoma formation.
To facilitate visualization of the infundibulum and porta hepatis, the assistant employs a toothed grasper to push the gallbladder’s fundus cranially and slightly laterally towards above the liver at 10 o’clock. The surgeon utilizes forceps to grasp the infundibulum’s left side, retracting it downward and to the side to create an optimal angle between the cystic duct and the common duct. This instrument serves to provide varying angles of retraction, enabling anterior and posterior views of the anatomical triangle. The dissection of the gallbladder-cystic duct junction commences with gentle peritoneal scraping, typically initiated above the gallbladder. A fundamental principle is to maintain dissection along a known safe structure, typically the gallbladder, to enhance the visualization of unfamiliar structures. The posterolateral aspect of the gallbladder is regarded as the safest region for initial dissection and can be exposed by retracting the infundibulum superiorly and medially. Unless the cystic duct is notably short, dissection down to the cystic duct-common bile duct junction is unnecessary. Following anterior and posterior dissection, the lower one-third of the gallbladder is separated from the liver, commencing from the infundibulum towards the fundus. All the dissection during the LC must be done ventral and cephalad to Rouviere’s sulcus (10). During this phase, the gallbladder should exhibit only two elements leading to the purse—a criterion known as the “critical safety view”—which must be met prior to any tubular structure division (Figure 3). Failure to achieve these goals warrants abstention from clipping any structures, and total cholecystectomy is not attempted (8). Similarly, the cystic artery is dissected. Calot’s lymph node is often adjacent to and anterior to the artery, serving as a useful landmark for locating the cystic artery. It is essential to remain cognizant of potential anatomical variations to prevent misidentification of structures. Subsequently, the proximal cystic artery is clipped, and the distal segment may be cauterized. The integrity of the cystic duct is verified by reconstructing it from anterior and posterior perspectives before closure with a clip and division with scissors. Following secure ligation and division of the cystic artery and duct, the gallbladder is separated from the liver bed toward the fundus, employing cautery. The gallbladder is then displaced to the right side of the liver, and hemostasis is ensured within the sac bed. Finally, the gallbladder is retrieved from the abdominal cavity through the entry point created by the epigastric or umbilical large-diameter trocar.
In this technique, called standard four ports, LC is usually performed with two pieces of 10 mm trocar and two pieces of 5 mm trocar as standard. However, in some difficult cases, in case of dense adhesion or insufficient exposure, an additional 5 mm port in the left hypochondrium for retraction of the duodenum or continuous suction during dissection in Calot’s triangle may be required. We present this article in accordance with the Narrative Review reporting checklist (available at https://ales.amegroups.com/article/view/10.21037/ales-23-54/rc).
Methods
The objective of this review is to analyze the technical evolution of LC since its inception, considering current literature. We searched original papers, reviews and meta-analyses published up to September 2023, about the technical development of laparoscopic surgery in the management of benign gallbladder diseases using PubMed. Relevant studies were identified using different combinations of the following search terms: “Laparoscopic cholecystectomy”, “Technical developments”, “Modified techniques”, “New technique”, “Cholelithiasis”, “Cholecystitis”, “Single incision laparoscopic surgery”, “Single site laparoscopic cholecystectomy”, “Mini-laparoscopic cholecystectomy”, “Robot-assisted cholecystectomy”, and “NOTES”. Additional papers were identified by reviewing reference lists of relevant publications. Publications with relatively low credibility and in languages other than English were excluded. We systematically categorized the modified methods based on the number of ports and subsequently examined each method individually. Meta-analyses and systematic review articles were predominantly utilized to compare outcomes across different methods, focusing on early-stage complication rates, procedure duration, postoperative pain, and hospital stay. More details of the method are shown in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | Sep 15, 2023 |
| Databases and other sources searched | PubMed |
| Search terms used | “Laparoscopic cholecystectomy” [MeSH] AND “Technical developments” [MeSH] |
| “Laparoscopic cholecystectomy” [MeSH] AND “Modified techniques” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “New technique” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “Cholelithiasis” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “Cholecystitis” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “Single incision laparoscopic surgery” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “Single site laparoscopic cholecystectomy” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “Mini-laparoscopic cholecystectomy” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “Robot-assisted cholecystectomy” [MeSH] | |
| “Laparoscopic cholecystectomy” [MeSH] AND “NOTES” [MeSH] | |
| Timeframe | 1980–2023 |
| Inclusion and exclusion criteria | The inclusion criteria encompassed full-text articles involving adults aged 18 years and older who underwent surgery with modified methods, distinct from the standard laparoscopic cholecystectomy, for benign gallbladder disease in both emergency and elective settings. Focus was placed on original papers, reviews and meta-analyses in English about modified and standard laparoscopic cholecystectomy surgical techniques for the treatment of benign gallbladder diseases |
| Publications with relative low credibility and non-English publications were excluded | |
| Selection process | It was conducted independently by H.S., T.K. and C.T.; all authors discussed the literature selection and obtained the consensus |
| Any additional considerations, if applicable | Some articles were identified by examining the reference lists of relevant publications, and some articles were already known to the authors before |
NOTES, natural orifice transluminal endoscopic surgery.
Modified LC techniques
The growing emphasis on cosmetology and flawless appearance in recent years has also influenced healthcare practices, including surgery. Surgeons have modified minimally invasive surgical techniques to make procedures less invasive and achieve better cosmetic results. While these modified methods have been shown to reduce postoperative pain and enhance cosmetic outcomes, it is crucial to ensure that they do not compromise the fundamental principles of LC. The safety of gallbladder surgery should always take precedence over cosmetic considerations. Therefore, it is recommended that modified LC procedures be performed exclusively by experienced surgeons on carefully selected patients (8). In cases where difficulties arise during the procedure, it is advisable not to persist but rather to prioritize patient safety over cosmetic outcomes.
A review of the literature reveals that standard LC has been modified using over 50 different technical variations. These modifications range from altering trocar sizes and placements to techniques.
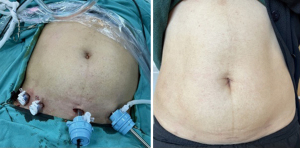
Four port modified LC techniques
One common approach in this category involves altering port sizes while maintaining the same number of ports. This may entail reducing port sizes from 10 to 5 mm or from 5 to 3- or 2-mm (8). Surgeons using a 5-mm telescope may reduce the size of the umbilical port, while those employing a 5-mm clip applicator may reduce the size of the epigastric trocar. Some surgeons have even opted to downsize 3-mm trocars. Notably, surgeons may select the umbilical or epigastric 10-mm trocar for ease of gallbladder removal, as the gallbladder, enclosed in an Endobag, is extracted from the abdomen at the procedure’s conclusion through the 10-mm trocar. Furthermore, some surgeons aim to achieve improved postoperative cosmetic results by placing all trocars below the bikini line without altering their size (11,12). This approach is sometimes employed for suitable patients in our clinic (Figure 3).
Three port modified LC techniques
The most common technique in this category involves omitting the port inserted from the anterior axillary line and using cranial traction on the gallbladder fundus (13). Surgeons typically use two 10-mm trocars and one 5-mm trocar. It has been reported that trocar sizes may vary without changing, and some surgeons even perform microlaparoscopic cholecystectomies using 3 mm trocars. The most intriguing technique in this group involves placing a traction suture on the gallbladder, pulling the fundus towards the lower right chest area, and performing cholecystectomy with just three ports. To prevent minor bile leakage during surgery, it is recommended to place a figure-eight suture in the fundus and apply gentle traction to prevent rupture of the gallbladder wall (8).
Two port modified LC techniques
In this technique, surgeons often use two traction sutures with two ports. One of these is placed in the fundus of the gallbladder, just like in the three-port technique, and the other is in the Hartman region of the gallbladder (14). This approach is frequently employed for suitable patients in our clinic and any two-port LC surgery performed by us has been shared as a video demonstrative purposes for readers (Video 1). Some surgeons may insert traction sutures through the port instead of placing them percutaneously, or may use special laparoscopic tools for traction. Cases have also been reported in which the instrument with traction applied to the Hartman was sent through the camera port. Cases have been reported in which the operation was performed through a total of two incisions, although the umbilical port location was revised to a handmade single port or ready-made glove port and the use of multiple tools was used. As mentioned before, there are many modified versions in the literature.
Single incision modified LC techniques
In this technique, surgeons reach the abdomen with a single incision from the belly button and enter all surgical instruments from the same place. While special single ports are used for this, some surgeons use handmade trocars. Nevertheless, single-incision robot-assisted cholecystectomy cases have also taken their place in the literature. There are also modifications to the single incisions seen in other methods. So much so that even cases of gasless have been reported without the use of CO2 infusion (15).
Needlescopic cholecystectomy
Surgeons utilized 2 mm special instrument instead of 5- and 10-mm trocars in all port locations, with the exception of the umbilical port, in standard LC and designated the technique as needlescopic cholecystectomy. This method involved the use of specialized graspers, scissors, and laparoscopes designed to operate through a 2-mm opening. During the clamping of the cystic artery and duct, a 2-mm laparoscope was employed the lateral port to visualize, while the clip applicator was inserted through the umbilical port (16). One drawback of this modification for surgeons aiming to minimize incisions and tissue trauma at the other three port sites is the necessity to use specialized equipment in this technique. Furthermore, there are authors who use needle graspers for gallbladder fundus traction in combination with single incision LC (17).
Robot-assisted cholecystectomy
Robotic surgical systems are progressively transforming the landscape of minimally invasive surgery, leading to the growing popularity of single-port cholecystectomy. Among the most prominent advantages associated with the utilization of robotic systems in various surgical procedures today are the provision of three-dimensional (3D) visualization, mitigation of instrument tremors, and enhanced instrument flexibility. Robot-assisted cholecystectomy can be executed through a single incision at the umbilicus or through multiport (18). Recent studies in the medical literature have undertaken a multitude of comparisons between conventional LC and robot-assisted cholecystectomy. A recurring consensus across the majority of these studies is the prolonged duration of the operation and the elevated cost associated with the robot-assisted approach (19). However, there are almost no studies in the literature comparing 3D imaging LC with robot-assisted cholecystectomy. 3D imaging provides 3D visualization and stereopsis similar to robot-assisted cholecystectomy (20). Its disadvantage lies in the lack of instrument articulation, but this does not pose a significant drawback for experienced surgeons performing cholecystectomy surgery. In the current literature to the best of our knowledge, 3D imaging LC is often compared with traditional LC and not with robot-assisted cholecystectomy. Although the results vary, the general opinion is that it shortens the operation time and reduces complication rates (21-23).
Natural orifice transluminal endoscopic surgery (NOTES) cholecystectomy
In this group, hybrid transvaginal methods are mainly used. Surgeons usually perform the surgery by inserting the first trocar from the umbilical region and inserting the other trocars transvaginally from the posterior fornix (8,24,25). While transvaginal standard laparoscopic instruments can be used in the surgery, there are also cases performed with an endoscope (8,24,25). Transgastric and transcolonic techniques are not yet widely used due to the risk of peritonitis and fistula development and the difficulties in closing the defect in the healthy organ. It is estimated that it will be used frequently at the levels that endoscopic robotic surgery will reach in the future.
Discussion
Standard versus modified LC techniques
Early-stage complications
The most common early complications following LC include BDI, bile duct leak, wound infection, intra-abdominal infection, etc. The most important of these complications is BDI. Although complication rates were higher than open cholecystectomy when LC was first described, this rate has decreased as surgeons’ laparoscopic skills have increased. According to our current knowledge BDIs have an estimated incidence of 0.4–1.5% (3). Many articles in the literature have compared methods in early-stage complications. A recently published meta-analysis, examining 17 randomized controlled trials, reported the lowest complication rate for three-port and standard LC (26). In another large-scale meta-analysis, it was noted that there was no difference between the methods regarding early postoperative complications, except for a lower rate of wound infection in needlescopic cholecystectomy (27). A meta-analysis comparing robot-assisted cholecystectomies with laparoscopic cholecystectomies found no difference in intraoperative and postoperative complications related to the method (19).
Length of procedure
When the methods were compared in terms of surgery time, it was seen that the shortest surgery time was in the three-port technique (26). However, there are also articles reporting that there is no difference in processing time between three-port methods and standard LC (28). In another study, it was published that the operating time in single-incision LC and needlescopic cholecystectomy was shorter than standard LC (27). Han et al. (19) examined robot-assisted cholecystectomy in benign gallbladder diseases and found that the surgery time was much longer than standard LC.
Postoperative pain
When standard LC and other methods are compared in terms of postoperative pain, the obvious superiority of the modified methods draws attention. In a study, it was determined that single-incision robot-assisted cholecystectomy was the method with the least postoperative pain, followed by other single-incision methods (26). Another study found that needlescopic was associated with minimal postoperative pain (27). Nevertheless, in a meta-analysis comparing randomized controlled trials comparing single-incision LC with multiple-port, no difference in postoperative pain was observed (28).
Length of hospital stay
Although the main goal of modified LC surgery is to improve cosmetic results, it is compared to standard LC in almost every respect. A recently published meta-analysis examining 18 studies involving 2,085 patients reported shorter hospital stay with three-port LC than with standard LC (29). In another meta-analysis including 17 randomized controlled studies comparing modified methods among themselves, it was reported that hospital stay times were shorter in single incision robot-assisted cholecystectomy and three-port LC (26). Another more comprehensive meta-analysis found that needlescopic cholecystectomy was associated with the shortest duration (27). According to the collective findings from these literature sources, modified methods are deemed advantageous in terms of reducing the length of hospital stays, even though this is not their primary goal. However, these studies did not delve into the impact of emergency or elective surgeries on the length of hospital stays. This was reported as a limitation since subgroup analysis could not be conducted. It is foreseeable that patients undergoing emergency procedures for acute cholecystitis will have longer hospital stays compared to elective cases, irrespective of the surgical method.
Conclusions
LC, following conventional cholecystectomy, has become a groundbreaking surgical treatment for benign gallbladder diseases. However, a similar consensus does not exist between standard LC and modified LC methods. Although some studies report advantages in certain aspects, there is no unanimous opinion as of yet. Regardless of the purpose when choosing the method, it is essential not to compromise on the principles of safe cholecystectomy and not to insist on modified methods in challenging cases. It should not be forgotten that switching to the open method after any iatrogenic biliary tract injury will increase the patient’s hospital stay and the need for postoperative pain relief. While seeking improved cosmetic results, one may have to make larger incisions.
Acknowledgments
We would like to show our gratitude to Ezgi Unlu who drew Figures 1,2 for the exceptional support with us during the preparation of this paper.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://ales.amegroups.com/article/view/10.21037/ales-23-54/rc
Peer Review File: Available at https://ales.amegroups.com/article/view/10.21037/ales-23-54/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ales.amegroups.com/article/view/10.21037/ales-23-54/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Reynolds W Jr. The first laparoscopic cholecystectomy. JSLS 2001;5:89-94. [PubMed]
- Warchałowski Ł, Łuszczki E, Bartosiewicz A, et al. The Analysis of Risk Factors in the Conversion from Laparoscopic to Open Cholecystectomy. Int J Environ Res Public Health 2020;17:7571. [Crossref] [PubMed]
- de'Angelis N, Catena F, Memeo R, et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg 2021;16:30. [Crossref] [PubMed]
- Strasberg SM, Eagon CJ, Drebin JA. The "hidden cystic duct" syndrome and the infundibular technique of laparoscopic cholecystectomy--the danger of the false infundibulum. J Am Coll Surg 2000;191:661-7. [Crossref] [PubMed]
- Strasberg SM, Gouma DJ. 'Extreme' vasculobiliary injuries: association with fundus-down cholecystectomy in severely inflamed gallbladders. HPB (Oxford) 2012;14:1-8. [Crossref] [PubMed]
- Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995;180:101-25. [PubMed]
- Jones RT, Sritharan M, Berry R. Comment on "Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy". Ann Surg 2021;274:e812. [Crossref] [PubMed]
- Haribhakti SP, Mistry JH. Techniques of laparoscopic cholecystectomy: Nomenclature and selection. J Minim Access Surg 2015;11:113-8. [Crossref] [PubMed]
- Kramp KH, van Det MJ, Totte ER, et al. Ergonomic assessment of the French and American position for laparoscopic cholecystectomy in the MIS Suite. Surg Endosc 2014;28:1571-8. [Crossref] [PubMed]
- Gupta V, Jain G. Safe laparoscopic cholecystectomy: Adoption of universal culture of safety in cholecystectomy. World J Gastrointest Surg 2019;11:62-84. [Crossref] [PubMed]
- Ersoz F, Ozcan O, Sari S, et al. Laparoscopic cholecystectomy on the bikini line for invisible scar. Surg Laparosc Endosc Percutan Tech 2011;21:e7-e10. [Crossref] [PubMed]
- Dursun A, Erdoğan E, Güler M. Safe and aesthetic; Laparoscopic cholecystectomy on the bikini line. Van Saglık Bilimleri Dergisi 2023;16:9-13. [Crossref]
- Kumar M, Agrawal CS, Gupta RK. Three-port versus standard four-port laparoscopic cholecystectomy: a randomized controlled clinical trial in a community-based teaching hospital in eastern Nepal. JSLS 2007;11:358-62. [PubMed]
- Karsıdag T, Aydın H, Savas A, et al. İki Port ile Laparoskopik Kolesistektomi. Endoskopik Laparoskopik & Minimal invaziv cerrahi dergisi, 11. Ulusal Endoskopik Laparoskopik Cerrahi Kongresi 2-6 Ekim 2013 Bildiri Özetleri. 2013, Volume 20. Available online: https://www.elcd.org/uploads/fileman/11_ulusal_endoskopik_laparoskopi.pdf
- Ishikawa M, Asanoma M, Tashiro Y, et al. Gasless single-port laparoscopic cholecystectomy. J Minim Invasive Surg 2021;24:152-7. [Crossref] [PubMed]
- Franklin ME Jr, Jaramillo EJ, Glass JL, et al. Needlescopic cholecystectomy: lessons learned in 10 years of experience. JSLS 2006;10:43-6. [PubMed]
- Komine O, Suzuki H, Watanabe M, et al. Single-incision laparoscopic cholecystectomy with an additional needle grasper: a novel technique. J Nippon Med Sch 2015;82:43-9. [Crossref] [PubMed]
- Lee EK, Park E, Oh WO, et al. Comparison of the outcomes of robotic cholecystectomy and laparoscopic cholecystectomy. Ann Surg Treat Res 2017;93:27-34. [Crossref] [PubMed]
- Han C, Shan X, Yao L, et al. Robotic-assisted versus laparoscopic cholecystectomy for benign gallbladder diseases: a systematic review and meta-analysis. Surg Endosc 2018;32:4377-92. [Crossref] [PubMed]
- Patel M, Hugh TJ. A Comparison of Three-Dimensional Visualization Systems and Two-Dimensional Visualization Systems During Laparoscopic Cholecystectomy: A Narrative Review. J Laparoendosc Adv Surg Tech A 2023;33:957-62. [Crossref] [PubMed]
- Tauriainen A, Biancari F, Tauriainen T. Comparative Analysis of Three-Versus Two-dimensional Imaging in Laparoscopic Cholecystectomy. World J Surg 2021;45:1370-5. [Crossref] [PubMed]
- Shaikh AR, Shaikh AA, Abbasi M. Short term outcomes of three dimensional versus two-dimensional laparoscopic cholecystectomy. Pak J Med Sci 2021;37:162-6. [PubMed]
- Davies S, Ghallab M, Hajibandeh S, et al. Three-dimensional versus two-dimensional imaging during laparoscopic cholecystectomy: a systematic review and meta-analysis of randomised controlled trials. Langenbecks Arch Surg 2020;405:563-72. [Crossref] [PubMed]
- Peng C, Ling Y, Ma C, et al. Safety Outcomes of NOTES Cholecystectomy Versus Laparoscopic Cholecystectomy: A Systematic Review and Meta-Analysis. Surg Laparosc Endosc Percutan Tech 2016;26:347-53. [Crossref] [PubMed]
- Yang E, Nie D, Li Z. Comparison of Major Clinical Outcomes Between Transvaginal NOTES and Traditional Laparoscopic Surgery: A Systematic Review and Meta-analysis. J Surg Res 2019;244:278-90. [Crossref] [PubMed]
- Lin H, Zhang J, Li X, et al. Comparative outcomes of single-incision laparoscopic, mini-laparoscopic, four-port laparoscopic, three-port laparoscopic, and single-incision robotic cholecystectomy: a systematic review and network meta-analysis. Updates Surg 2023;75:41-51. [Crossref] [PubMed]
- Zhao JJ, Syn NL, Chong C, et al. Comparative outcomes of needlescopic, single-incision laparoscopic, standard laparoscopic, mini-laparotomy, and open cholecystectomy: A systematic review and network meta-analysis of 96 randomized controlled trials with 11,083 patients. Surgery 2021;170:994-1003. [Crossref] [PubMed]
- Lyu Y, Cheng Y, Wang B, et al. Single-incision versus conventional multiport laparoscopic cholecystectomy: a current meta-analysis of randomized controlled trials. Surg Endosc 2020;34:4315-29. [Crossref] [PubMed]
- Nip L, Tong KS, Borg CM. Three-port versus four-port technique for laparoscopic cholecystectomy: systematic review and meta-analysis. BJS Open 2022;6:zrac013. [Crossref] [PubMed]
Cite this article as: Sevik H, Karsidag T, Tatar C. A narrative review of technical developments for the laparoscopic cholecystectomy. Ann Laparosc Endosc Surg 2024;9:14.



