Complete bursectomy in totally laparoscopic total gastrectomy with D2 lymph node dissection for advanced gastric cancer
Introduction
Recently, the Chinese Laparoscopic Gastrointestinal Surgery Study (CLASS) group conducted several multicenter studies on the feasibility, safety and oncologic outcomes of laparoscopic gastrectomy for advanced gastric cancer (AGC) (1-3). And the findings were comparable to the conventional open surgery. On the other hand, interim analysis results of a randomized controlled trial suggest that bursectomy might improve survival (4). However, intracorporeal Roux-en-Y anastomosis and complete bursectomy are more difficult procedures during laparoscopic total gastrectomy. Based on membrane anatomy, we successfully performed complete bursectomy in totally laparoscopic total gastrectomy (TLTG) and Roux-en-Y esophagojejunostomy. Here we describe our experience and skills.
Methods
Patient
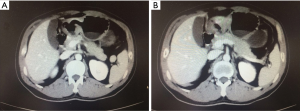
In this video (Figure 1), we performed complete bursectomy in TLTG Roux-en-Y esophagojejunostomy in a 41-year-old man with a malignant ulcer on body of stomach, and suspected the presence of cT3N1M0 gastric cancer (Figure 2).
Surgical procedure
The patient was placed in the supine position with legs apart under general anesthesia, and the operator stood on the left side of him. A 12-mm trocar was installed through a wound above the umbilicus for a 30-degree laparoscope. Pneumoperitoneum was established with carbon dioxide (CO2) and the intra-abdominal pressure was maintained at a constant 12 to 15 mmHg. Another 12-mm trocar was inserted in the left preaxillary line 12 mm below the costal margin as a major hand port, and a 5-mm trocar was inserted in the left midclavicular line 5 mm above the umbilicus as an accessory port. Then another two 5-mm trocars were placed at the contralateral site. After abdominal exploration, complete bursectomy with D2 lymphadenectomy was performed according to lymph node classification by the 4th Japanese Gastric Cancer Treatment Guideline. The duodenum was transected about 2 cm distal from the pylorus while the resection line of the esophagus was set as at least 5 cm off the tumor. Both of the performances used a 60-mm endoscopic linear stapling device, and the resected specimen was placed in a plastic bag. Following these procedures, Roux-en-Y anastomosis was processed with endoscopic linear stapling devices. An esophago-jejunal anastomosis was constructed at the point 20 cm distal to the Teritz ligament, and the stump was closed with endoscopic linear stapling device. After that, jejuno-jejunal anastomosis was performed using linear staplers at 40 cm distal to the esophagojejunostomy. Finally, by extending the incision of the umbilical port to 4 cm in the shape of a ‘C’, the specimen was extracted out.
Tips
Firstly, as membrane anatomy described, anterior lobe of transverse mesocolon and capsule of pancreas compose the partial anterior and posterior of bursa omentalis. In order to radically resect omental bursa, we should peel these two membranes. Fortunately, while doing this, several important vessels and lymph nodes would be separated at the same time. Secondly, in order to avoid stricture when closing the common entry hole in esophagojejunostomy and jejunojejunostomy, we prefer to use 60-mm endoscopic linear stapling devices to finish the anatomosis.
Results
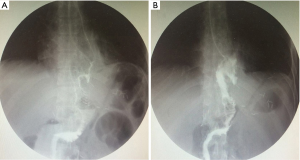
The operation time was 260 min with bleeding of about 50 mL. There were no intraoperative and postoperative complications happened. And the pathology result judged it as the signet-ring cell carcinoma staging T3N2M0 with 5/40 lymph nodes positive. Moreover it showed clear passageway and good motility with gastroenterography after operation (Figure 3), and the patient discharged from hospital on the 7th day.
Discussion
Gastric cancer is one of the most common malignancies in the world, and surgical resection remains the only curative treatment option. Although laparoscopic gastrectomy has gained popularity in treating early stage gastric cancer, there is a great deal of controversy surrounding the issue of safety and feasibility of it in AGC. Unfortunately, more than 80% of gastric cancer patients are diagnosed at advanced stages in China. Now, three famous multicenter RCTs are ongoing to compare laparoscopic gastrectomy with conventional open surgery for AGC. We are looking forward to the results, but as reported currently laparoscopic gastrectomy can be safely performed in AGC by experienced surgeons (1). What’s more, with improved cosmesis and faster recovery, intracorporeal anastomosis is thought to be a valid reconstruction method after gastrectomy (6). Besides, another controversial issue is whether it is worthy to perform bursectomy in all AGC patients. According to the Japanese Gastric Cancer Treatment Guideline, it is recommended for tumors with invasion of the serosa to avoid injury of transverse colon vessels and pancreas (7). But as revealed, this operation might decrease peritoneal recurrence and improve survival. Moreover, it won’t increase the risk of pancreatic fistula (4). In our department, we perform D2 lymph node dissection with bursectomy as common for gastric cancer these years. And it doesn’t find any different complication rates as others. What we favor is that it can fine a more clearly anatomic layer in performing bursectomy based on membrane anatomy.
Conclusions
It found that complete bursectomy in TLTG with intracorporeal Roux-en-Y esophagojejunostomy would be a safe and feasible surgical method with minimal invasiveness. So we suggest that this operation might be a better choice for gastric cancer in the experienced center.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2016.08.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hu Y, Huang C, Sun Y, et al. Morbidity and Mortality of Laparoscopic Versus Open D2 Distal Gastrectomy for Advanced Gastric Cancer: A Randomized Controlled Trial. J Clin Oncol 2016;34:1350-7. [Crossref] [PubMed]
- Hu Y, Ying M, Huang C, et al. Oncologic outcomes of laparoscopy-assisted gastrectomy for advanced gastric cancer: a large-scale multicenter retrospective cohort study from China. Surg Endosc 2014;28:2048-56. [Crossref] [PubMed]
- Yu J, Hu J, Huang C, et al. The impact of age and comorbidity on postoperative complications in patients with advanced gastric cancer after laparoscopic D2 gastrectomy: results from the Chinese laparoscropic gastrointestinal surgery study (CLASS) group. Eur J Surg Oncol 2013;39:1144-9. [Crossref] [PubMed]
- Fujita J, Kurokawa Y, Sugimoto T, et al. Survival benefit of bursectomy in patients with resectable gastric cancer: interim analysis results of a randomized controlled trial. Gastric Cancer 2012;15:42-8. [Crossref] [PubMed]
- Zang W, Teng W. Complete bursectomy in TLTG. Asvide 2016;3:347. Available online: http://www.asvide.com/articles/1116
- Han G, Park JY, Kim YJ. Comparison of short-term postoperative outcomes in totally laparoscopic distal gastrectomy versus laparoscopy-assisted distal gastrectomy. J Gastric Cancer 2014;14:105-10. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2016; [Epub ahead of print].
Cite this article as: Zang W, Teng W. Complete bursectomy in totally laparoscopic total gastrectomy with D2 lymph node dissection for advanced gastric cancer. Ann Laparosc Endosc Surg 2016;1:3.