
Enhanced recovery after surgery in elderly and high-risk patients
Introduction
The population >65 years of age in western countries has increased significantly in recent years, and the trend is still growing. More older patients will present with surgical disease and will need surgery. There is a considerable variability in physiological reserve in elderly patients and therefore biological, rather than chronological age, should be considered when evaluating these patients. However, age-related factors (such as reduced physical function and frailty) seem to be important predictors of adverse surgical outcomes (1).
Most older patients will do as well as their younger counterparts after elective surgery. However, 30-day mortality rate is still high among the oldest, and it continues to increase causing a higher 1-year mortality rate in these patients. Almost 40% of patients can develop postoperative complications, and 45% of these will be major complications (1). In a recent population-based study from Finland, severe complications were the only patient-related factor that had a significant effect on 1-year mortality (OR 9.60, 95% CI: 2.33–39.55, P=0.002). Severe complications were more common in patients who had a prior history of increased preoperative hospitalizations (31% vs. 15%, P=0.05), and in those who lived in nursing homes (30% vs. 17%, P=0.05) (2).
This shows that patients who have a decrease in physical and mental resources had more severe postoperative complications, and a higher mortality rate. It therefore seems that limited performance status, cardiopulmonary problems and surgery-related issues are the main factors contributing to 1-year mortality (3).
Frailty has appeared as an essential factor to evaluate in preoperative assessment, primarily because it has been independently associated with increased morbidity and mortality after surgery (4-7). We still do not know what the gold-standard measurement tool for frailty is. It is usually been considered as one of the geriatric syndromes, along with sarcopenia and cachexia. Increasing age is correlated with increased frailty, although frailty can appear in other age groups. Frailty is a pathophysiological process that involves an interaction of physical inactivity, endocrine changes, inflammatory reaction, autonomic instability, and poor nutrition. These aspects result in a decreased muscle mass and sarcopenia, which forms an important aspect of frailty. Interventions that are designed to treat reversible conditions (including congestive cardiac failure and chronic renal failure) could be effective in reducing, or even reversing, frailty. Therefore, a preoperative evaluation of the patient’s physical and cognitive performance focusing on preoperative cardiopulmonary status and medical optimization becomes important in these patients (7).
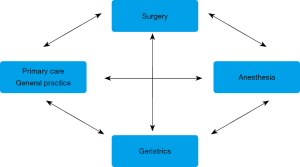
Surgery can be especially risky for frail patients and could activate an irreversible functional decline (8). Quality care for older adult surgical patients should produce outcomes consistent with patient goals and requires clear communication and coordination from many health professionals. To deliver high-value care in elderly patients, a reliable hospital system, with a clear safety culture, and well-synchronized care with readily available care protocols is necessary (9). A multidisciplinary pathway of care including individualized evaluation by geriatricians, anesthesiologists, surgeons and other specialists to detect frailty and other risk factors for functional decline can improve outcomes in these patients. The Comprehensive Geriatric Assessment (CGA) has been shown to be useful in elective surgery in elderly high-risk patients, and can potentially help to reduce post-operative complications and length of stay (LOS) (6).
Enhanced recovery after surgery (ERAS) and prehabilitation are an attractive combination that could improve the baseline condition of frail patients; these pathways could potentially increase the ability of these patients to withstand the stresses of surgery.
Prehabilitation in elderly and high-risk patients
ERAS protocols are increasingly used to improve surgical outcomes. These evidence-based perioperative protocols have been used in several specialties such as colorectal surgery, thoracic surgery, gynecologic surgery, and urology, with an improvement in clinical results (10).
ERAS programs are designed to cover preoperative, intraoperative and postoperative stages, and focus on providing an optimal recovery for patients. They vary depending on the type of surgery and usually include optimization of nutritional status, anemia, mobility, early feeding and analgesia (11).
The concept of prehabilitation has emerged as an increasingly important part in the preoperative phase of ERAS (12). Prehabilitation should be included after the indication for surgery is established and used before hospital admission and surgery. The relevant concepts of prehabilitation are the ability to adapt to physical stress and preservation or even enhancement of physiological reserve. The muscle groups most affected by inactivity, bed rest or immobilization are those used for ambulation. Prehabilitation may be especially useful to improve the physical function of high-risk patients during the preoperative period. It could (partly) prevent the deterioration of the cardiovascular, respiratory or musculoskeletal systems, and therefore lower the risk of postoperative morbidity and mortality. Prehabilitation programs include different interventions including physical training, psychological council and exercises in “mindfulness” and nutritional supplements. Because frail patients are more vulnerable to surgery, prehabilitation might be especially beneficial in this patient group (13). Elderly patients with comorbidities are prone for perioperative complications and, consequently, they should be the most likely to benefit from prehabilitation programs. A full CGA or geriatric evaluation could also be included in the prehabilitation plan to improve outcomes in the elderly, if the necessary preoperative actions can be implemented. Geriatric care includes optimization of the patient´s medication, pain management, early mobilization, delirium prevention and careful screening and management of other medical complications.
A recent randomized controlled study of prehabilitation including 125 high-risk patients (62 in the personalized prehabilitation arm vs. 63 controls) found a 51% reduction in postoperative complications. The prehabilitation program included 3 interventions: a motivation consultation, endurance high-intensity training, and promotion of physical activity. Patients also followed an ERAS program. The main finding of the study showed that prehabilitation was a protective factor for postoperative complications in high-risk candidates for elective major abdominal surgery (14).
Another recent study focused on the possible effect of prehabilitation on the rates of postoperative delirium (15). This single center uncontrolled before-and after study included patients >70 (360 control patients and 267 prehabilitation patients). All patients also followed an ERAS program. The program was designed to improve overall health, and included exercises to be performed at home, nutritional advice and intravenous iron infusions when anemia was detected. In case of frailty a geriatrician performed a CGA and provided additional preoperative interventions when deemed necessary. The authors concluded that elderly patients that underwent elective major abdominal surgery (AAA or colorectal cancer), could have a decrease in the incidence of postoperative delirium by implementing a prehabilitation program during the pre-admission period. This program should focus on optimizing patient´s fitness and nutritional status, and treatment of anemia and frailty issues. However, the authors did not find a reduction in LOS, number and length of unplanned ICU admissions, and rates of other postoperative complications.
The evidence for prehabilitation is still not robust. Most studies are small, and the programs are heterogeneous (13). For frail patients, probably a combination of inspiratory muscle training, nutritional optimization, and cognitive exercises is the future, although further studies are needed (13). It should also include a more holistic focus, including management of patients with multiple medications, optimization of chronic comorbidities, and any modifications of the home to optimize functional status.
ERAS and the elderly or high-risk patient
ERAS programs are pathways of care that include combinations of evidence-based changes in preoperative, intraoperative, and postoperative care with the aim of reducing organ dysfunction and surgical stress response to surgery (11). ERAS guidelines include mostly between 15–20 perioperative elements. The key elements seem to be extended patient information, conservation of gastrointestinal function (carbohydrate solution before surgery, early enteral feeding), minimizing surgical trauma and postoperative organ impairment (goal-directed fluid therapy, avoidance of drains and nasogastric tubes, minimally invasive surgery), proactive pain management (opioid sparing anesthesia and analgesia, local anesthetic infiltration of incisions) and early mobilization to promote patient autonomy (11,12,16).
ERAS implementation involves a team consisting of surgeons, anesthesiologists, an ERAS coordinator, and staff in the preoperative evaluation clinic, pre-anesthesia-holding area nurse, operating room nurse, as well as staff in the surgical ward and/or the intensive care unit (12).
Multiple studies have shown that ERAS protocols reduce the LOS in most major surgical procedures, without associated increases in mortality, complications or readmissions. There are some logistical challenges in older patients, however, such as the home care situation. Elderly patients might not be fit enough to go home even when discharge criteria are fulfilled, and they may have to wait for nursing home placement. Therefore, LOS may not be reduced as significantly as in younger patients (17,18).
The safety of ERAS in older patients has been extensively reviewed in recent studies (17,18). The European Society of Anesthesiology recommends the use of ERAS surgery as an adjunct in the prevention of postoperative delirium in high-risk patients (19), and perioperative NSQIP recommendations include many of the ERAS items to be used in geriatric patients, such as limiting fasting, avoiding opioid use, early mobilization, and early oral intake to decrease complications (20).
In a recent systematic review of 21 articles on the efficacy of ERAS in elderly patients between 2000–2015, the authors included 16 studies; 4 compared the efficacy of ERAS compared to traditional management in the elderly. Three randomized studies were included; the groups were comparable by population, but all had methodological flaws. ERAS protocols presented a significant benefit with regards to shorter duration of hospitalization (7 vs. 12 days), fewer overall complications (5% vs. 21%), and a decrease in postoperative morbidity by 45%. They concluded that ERAS is feasible in the elderly, and the benefits are comparable to younger patients. Postoperative morbidity remains higher in the elderly compared to younger patients, but all the studies showed that ERAS reduced complications in elderly patients when compared to traditional management (21).
The ERAS measures that have shown benefit in elderly and high-risk patients include preoperative planning, with extensive and individualized information, education and post-discharge arrangements, screening for frailty and prior medical conditions, optimization of these conditions and of anemia, and special attention to delirium prophylaxis. In the intraoperative phase, attention should be given to maintain body temperature, multimodal analgesia using epidural or locoregional anesthetic techniques, avoidance of nasogastric tubes and drains, and the use of minimally invasive surgery whenever possible. Postoperatively, these patients benefit from a prompt return of personal sensory aids (glasses, walking aids, etc.); early mobilization, early removal of urinary catheters, and a proactive avoidance of postoperative nausea and vomiting, which could be a risk factor for aspiration (9,16-18).
Conclusions
Older patients are more likely to have a greater number of comorbidities, and also functional and cognitive impairment, polypharmacy, and disabilities. In these patients it is especially important to select the most appropriate surgical procedure and optimize functional status to prevent postoperative complications: minimally invasive surgery, prehabilitation, and ERAS programs can be beneficial in these patients.
Most of the published studies show that ERAS is possible in elderly patients, and presents similar results to younger patients (17,18,21). Biological characteristics should be the basis of treatment decisions and choice of surgical procedure, and not chronological age. By spending extra time identifying and treating conditions that can be improved in complex patients, we may be able to decrease postoperative complications and length of hospital stay. High levels of compliance with ERAS interventions can be obtained when a dedicated multidisciplinary team is involved in the care of these high-risk patients. Even if they are less compliant than younger patients, they seem to benefit just the same, even if they require longer convalescence after major surgery.
Patient-centered multidisciplinary models that include an assessment of frailty, the collaboration of geriatric medicine, primary care, and a focused pathway of prehabilitation, perioperative and postoperative management should be further investigated as the optimal management of elderly and high-risk patients undergoing surgery (Figure 1).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Corrado Pedrazzani) for the series “Enhanced Recovery After Gastrointestinal Cancer Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. This article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales.2020.02.05). The series “Enhanced Recovery After Gastrointestinal Cancer Surgery” was commissioned by the editorial office without any sponsorship or funding. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Byrnes A, Banks M, Mudge A, et al. Enhanced Recovery After Surgery as an auditing framework or identifying improvements to perioperative nutrition care of older surgical patients. Eur J Clin Nutr 2018;72:913-6. [Crossref] [PubMed]
- Niemeläinen S, Huhtala H, Ehrlich A, et al. Risk factors of short-term survival in the aged in elective colon cancer surgery: a population-based study. Int J Colorectal Dis 2020;35:307-15. [Crossref] [PubMed]
- Olotu C, Weimman A, Bahrs C, et al. The perioperative care of older patients. Dtsch Ärztebl Int 2019;116:63-9. [PubMed]
- Milder DA, Pillinger NL, Kam PCA. The role of prehabilitation in frail surgical patients: A systematic review. Acta Anaesthesiol Scand 2018;62:1356-66. [Crossref] [PubMed]
- Subramaniam A, Tiruvoipati R, Lodge M, et al. Frailty in the older person undergoing elective surgery: a trigger for enhanced multidisciplinary management. ANZ J Surg 2020;90:222-9. [Crossref] [PubMed]
- Chan SP, Ip KY, Irwin MG. Peri-operative optimization of elderly and frail patients: a narrative review. Anaesthesia 2019;74:80-9. [Crossref] [PubMed]
- Ko FC. Preoperative frailty evaluation: a promising risk-stratification tool in older adults undergoing general surgery. Clin Ther 2019;41:387-99. [Crossref] [PubMed]
- Audisio RA. Tailoring surgery to elderly patients with cancer. Br J Surg 2016;103:e10-e11. [Crossref] [PubMed]
- Berian JR, Rosenthal RA, Baker TL, et al. Hospital Standards to promote optimal surgical care of the older adult. A report from the Coalition for Quality in Geriatric Surgery. Ann Surg 2018;267:280-90. [Crossref] [PubMed]
- Dworsky JQ, Castle SC, Lee CC, et al. Gerofit prehabilitation pilot program: preparing frail older veterans for surgery. J Healthc Qual 2019;41:91-8. [Crossref] [PubMed]
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-8. [Crossref] [PubMed]
- Iqbal U, Green JB, Patel S, et al. Preoperative patient preparation in enhanced recovery pathways. J Anaesthesiol Clin Pharmacol 2019;35:S14-23. [PubMed]
- McIsaac DI, Jen T, Mooker N, et al. Interventions to improve the outcomes of frail people having surgery: A systematic review. PLoS One 2017;12:e0190071 [Crossref] [PubMed]
- Barberán-Garcia A, Ubré M, Roca J, et al. Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery. A randomized blinded controlled trial. Ann Surg 2018;267:50-6. [Crossref] [PubMed]
- Janssen TL, Steyerberg EW, Langenberg JCM, et al. Multimodal prehabilitation to reduce the incidence of delirium and other adverse events in elderly patients undergoing elective major abdominal surgery: an uncontrolled before-and-after study. PLoS One 2019;14:e0218152 [Crossref] [PubMed]
- Braga M, Pecorelli N, Scatizzi M, et al. Enhanced recovery program in high-risk patients undergoing colorectal surgery: results from the perioperative Italian society registry. World J Surg 2017;41:860-7. [Crossref] [PubMed]
- Slieker J, Frauche P, Jurt J, et al. Enhanced recovery ERAS for elderly: a safe and beneficial pathway in colorectal surgery. Int J Colorectal Dis 2017;32:215-21. [Crossref] [PubMed]
- Millan M, Renau-Escrig AI. Minimizing the impact of colorectal surgery in the older patient: The role of enhanced recovery programs in older patients. Eur J Surg Oncol 2020;46:338-43. [Crossref] [PubMed]
- Aldecoa C, Bettelli G, Bilotta F, et al. European society of anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 2017;34:192-214. [Crossref] [PubMed]
- Mohanty S, Rosenthal RA, Russell MM, et al. Optimal perioperative management of the geriatric patient: a best practices guideline from the American College of Surgeons NSQIP and the American Geriatric Society. J Am Coll Surg 2016;222:930-47. [Crossref] [PubMed]
- Launay-Savary MV, Mathonnet M, Theissen A, et al. GRACE (Groupe francophone de Réhabilitation Améliorée après Chirurgie). Are enhanced recovery programs in colorectal surgery feasible and useful in the elderly? A systematic review of the literature. J Visc Surg 2017;154:29-35. [Crossref] [PubMed]
Cite this article as: Millan M. Enhanced recovery after surgery in elderly and high-risk patients. Ann Laparosc Endosc Surg 2020;5:39.


