Definitions and current indications for obesity and metabolic surgery
IntroductionOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
In 1950s, the jejunoileal bypass (JIB) surgery, the earliest method of Obesity and Metabolic Surgery, was chosen as an effective treatment for weight loss and dyslipidemia. During these initial operations, with an anastomosis between proximal jejunal segments and distal ileal segments, most of the small intestines were bypassed (1). Despite modifications to the procedures performed, the malabsorbtive procedures became debatable and generally not accepted by Surgical Societies, due to serious metabolic post-JIB side effects. In 1966, Dr. Mason introduced the first gastric bypass operation, which initially was with horizontal gastric transection and Loop ileostomy (2). However, due to different complications, mostly due to biliary reflux, the Bypass operation is evolved into its current standard format of Roux-en-Y loop, that has now been used for many years (3-5).
Restrictive operations concept was progressed from vertical banded or stapled gastroplasties, to gastric band operations that were very popular in 1990s (6,7). There have been numerous arguments about different types of operations and different overall effects. Restrictive and malabsorbtive operations are still being discussed and more recently some surgeons prefer not to divert the operations in two different pathways as, restrictive and/or malabsorbtive.
Current concepts of Bariatric and Metabolic Surgery operations and recent metabolic studies reveal that, the mechanisms of these operations seem to extend beyond the magnitude of weight loss. Everyday researchers are working on different hormonal pathways that could be responsible for the early metabolic improvements, especially weight–independent glucose-lowering effects of Bariatric and Metabolic Surgery (8). When the evolution of the Bariatric and Metabolic Surgery operations are inspected, one can see that from the very beginning, the early metabolic positive effects thrilled the researchers more than the final weight loss success, which was in fact the main goal. However, the mid- to long-term side effects like malabsorption of nutrients, made researchers and surgeons to further seek for more innovative Bariatric and Metabolic operations with fewer complications.
Current accepted operations like sleeve gastrectomy (SG), Gastric Bypass and others, promise maximum weight loss and metabolic regulatory effects with minimum complication rates. Controlled randomized studies that were performed especially in the last decade and the Bariatric and Metabolic Societies that supported the literature with guidelines, strengthen the concept of metabolic surgery. Current guidelines support the use of metabolic surgery in individuals with mild obesity and uncontrolled Type 2 Diabetes Mellitus (T2DM) (9,10).
Definitions of bariatric & metabolic surgeryOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
Prevalence
Obesity is one of the major public health problems for modern world. It affects people at any age and from all kind of social, economical and cultural backgrounds. Obesity and obesity related chronic diseases including, cardiovascular disease, diabetes, metabolic syndrome, and many cancers are increasing globally. The data about worldwide health trends between 1980 and 2013 showed that, obesity-related deaths are three times more than fatalities related to malnutrition and starvation (11).
A comprehensive research made by World Health Organisation (WHO) in 2016 identified that; 39% of adult men and women (aged +18) with a BMI >25 kg/m2 were “overweight”. Further 11% of men and 15% of women with BMI >30 kg/m2 were “obese”. In the same year, the research showed that 18% of children and adolescents were overweight or obese. According to WHO, it is certain that obesity has increased dramatically over the past quarter of the century. WHO research identifies that the obesity epidemic is affecting more than 10% of the whole world population and it is now introduced as “Globesity” in order to emphasize its threat for the global health (12).
While obesity rates are increasing, the operations performed annually are also increasing. In the 2013 survey of International Federation for the Surgery of Obesity and Metabolic Diseases (IFSO), the total number of bariatric procedures performed worldwide was 468,609. The most commonly performed procedure in the world was Roux-en-Y gastric bypass (RYGB) with 45%, followed by sleeve gastrectomy (SG) with 37%. However, currently, SG is reported to be the most frequently performed procedure in the United States of America and Canada (13). According to American Society of Bariatric and Metabolic Surgery (ASMBS), SG operations performed in the USA weighted nearly 60% of the whole bariatric and metabolic surgery procedures that was performed on 2016 and 2017. While RYGB rates decreased from 35% to 18% between 2011–2017 (14).
Surgical procedures
SG
SG is a procedure that is performed by removing about 80% of the stomach and resizing the remnant stomach in a ‘banana shape’ tube form.
SG is technically simpler than the other malabsorbtive procedures. This technique was found to cause fewer major complications within the first month of the post-operative period (15). ASMBS defines SG as a recognizable primary surgical procedure for patients who was planned a staged approach. There are some technical concerns regarding the procedure and its long-term results that should be interpreted carefully. First of all, as SG is a restrictive operation with an increased post-operative intraluminal pressure, the operation choice in preoperative gastroesophageal reflux disease is debatable. Moreover, there is strong evidence that SG is shown to increase post-operative reflux or de novo reflux (16,17). Therefore, when considering indications of surgery, reflux is not a strong contraindication however, one should know that with current data in patients with reflux disease that was diagnosed preoperatively, the operation of choice should be the RYGB procedure. RYGB is shown to be effective on resolving GER symptoms (18,19).
Another concern regarding SG’s long-term results show major decrease of %EWL that could result in weight regain (from starting %EWL of 80% to 50–60% in 5 years) and showed around 20% remission rate of diabetes, within 5 years (20,21). In malabsorbtive operations such as RYGB, the remission rate of DM and long term EWL success is slightly better. This does not make SG a less successful operation but the need for further investigation still remains, in order to improve long term results about the procedure. Despite this, SG is still the most performed operation in the USA and rising in whole world of Bariatric Surgery.
RYGB
The RYGB is one of the most common and oldest weight-lost procedures in the world. The operation has been performed for over 30 years.
In this procedure, the surgeon makes a small pouch of about 30–40 mL from the proximal stomach and attaches this pouch to jejunum that is called a roux limb. There is a second anastomosis that provides connection between the residue stomach and duodenum to ileum. The general preference of distance between anastomosis differs with wide spectrum from 50 to 150 cm. The aim of this procedure is to bypass the large part of the stomach and duodenum. The gastric bypass works by several mechanisms. Firstly, similar to most bariatric procedures, the newly created stomach pouch is considerably smaller and this restrictive effect facilitates significantly smaller meals, which translates into fewer calories consumed. Additionally, as there is less digestion of food through the smaller stomach pouch, and there is a segment of small intestine that would normally absorb calories as well as nutrients that no longer has food going through it, there is probably to some degree less absorption of calories and nutrients.
Most importantly, the rerouting of the food stream produces changes in the gut hormones that promotes satiety, suppresses hunger, and reverses one of the primary mechanisms by which obesity induces T2DM. Long term weight loss results and T2DM remission is slightly better in RYGB surgery when compared with SG.
However, strong data showed that RYGB surgery has slightly higher rates of early complications, such as infectious complications and hemorrhage (22). Moreover, after and RYGB, internal hernia that weights around 10% of patients remains to be another big concern. In the long-term, vitamin and mineral deficiencies of vitamin B12, folate, zinc, iron, copper, calcium, and vitamin D, are slightly higher in bypass surgery when compared to SG (23,24).
Compared with open GBP, laparoscopic GBP was associated with a decrease in the frequency of iatrogenic splenectomy, wound infection, incisional hernia, and mortality; however, there was an increase in the frequency of early and late bowel obstruction, gastrointestinal tract hemorrhage, and stomal stenosis (25). Despite the minimal increased rate of complications of RYGB and uptrend of SG, RYGB surgery is still preferred for some patients and surgeons.
Adjustable gastric band
The adjustable gastric band is a weight-loss procedure that involves the placement of a band around the upper portion of the stomach. It is a strongly criticized procedure by surgeons because of its long-term results and mid-long term complications. Remission of diabetes occurs in approximately in 45–60% of patients. The remission or improvement of diabetes however, is secondary to the weight-loss produced by the procedure and there does not appear to be any other mechanism for diabetes improvement in band patients. This is one of the downsides of this operation. In other words, patients who have diabetes and who are unsuccessful in losing weight with the AGB will unlikely see any improvement in the diabetes.
There are studies with good and even long-term weight loss effects of LAGB in literature. However, most studies show that LAGB does not provide favorable results, especially in the long term. In early post-operative period the %EWL over 50% success rate weighted even more than 60% of the patients. Yet, when it comes to long-term results, most of the studies show that overall weight loss success rate decreased to less that 20% (26). Moreover, LAGB complication rates and long-term re-operation rates are high and most of the experts are now against LAGB surgery and not performing it in their surgical practices (27,28).
On the other hand, there are couple of authors that still use and favor new types of gastric band in their selected patients. Banded bypass is one of the new procedures that a gastric band is combined with RNY bypass surgery. This procedure is aimed to lower the long-term weight regain after standard gastric bypass surgery. Couples of studies show that with this type of procedure, long-term weight loss results are statistically better when compared to conventional Bypass procedure (29).
Gastric band procedures are generally described as a medical tale that gone wrong however still creates interest on surgeons with new procedural variations and newer types of devices.
Duodenal switch
The Duodenal Switch is a malabsorptive procedure performed far less frequently than the gastric bypass, SG or the adjustable gastric band, due to its procedural complexity and the greater risk of complications. Studies find however, that the operation is the most effective in inducing early and sustained remission or improvement in T2DM (more than 85% remission rates with weight-loss independent effects).
Possible additive results and features of both SG and Gastric Bypass operations are theoretically combined with the DS surgery (30,31). SG is the first part of the procedure. Then duodenal transection is performed and duodenoileal anastomoses is performed 250–300 cm proximal from the ileocecal junction. Both restrictive and malabsorbtive effects are combined with this procedure. Patient selection is generally diabetic patients with extremely high BMI. A 2-step procedure is also possible with the first operation—a SG and 6–18 months later 2nd step of bypass might be performed. Long-term %EWL results are at a remarkable rate around 80–100% and diabetes remission is around 90%. However, mid-long term malabsorption of the micronutrients is a troublesome complication of this procedure. There are studies of the DS that report superior weight loss and improvement of major comorbidities when compared to other operations. On the other hand, reports mostly show that complication and adverse event rates are similar to those of RYGB (32,33).
One anastomosis bypass (mini-gastric bypass)
One anastomosis bypass was first performed in 2001. The procedure involves re-sizing the stomach in a tube form and anastomosis the small intestine bypassing 200 cm of the upper part to the tube stomach. The advantage of a mini gastric bypass is the simplicity when compared with RNY gastric bypass, as it minimizes the operation time and related complications. Long-term weight loss and metabolic benefits are found to be sufficient and slightly better when compared to SG, and even RNYGB on some occasions. But there are some possible downsides and concerns such as the potential cause of bile reflux and ulcer, which have a negative influence on a patient’s quality of life. Another debate on one anastomosis gastric bypass (OAGB) is the biliopancreatic (BP) limb length. The BP limb length that was described in the original OAGB was 200 cm (34,35). However, there are some concerns about malabsorption therefore the consensus statements of OAGB is indecisive on the recommended BP limb length. OAGB has passed an obstacle when the IFSO has agreed to determine whether MGB-OAGB is an effective and safe procedure and whether it should be considered as a surgical option for the treatment of obesity and metabolic diseases. IFSO also agreed about the standard nomenclature should be the mini gastric bypass-OAGB (36,37).
Other procedures
Single anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) is a modified bariatric procedure of the BP diversion. The procedure includes SG and one anastomosis between stomach and the small intestine that 250 cm from ileocecal valve.
Especially patients with insulin dependent diabetes and have a BMI more than 50 should consider this procedure. However, major nutrient deficiencies can appear after SADI-S (38).
There are other obesity and metabolic operations that has gained interest over the last decade. SG with Transit Bipartition (TB), Single Anastomosis Sleeve Ileal Bypass (SASI) and SG with Ileal Interposition are other types of operations, which have been performed less, yet attract attention for future research. Their roles on obesity and related diseases are still being evaluated.
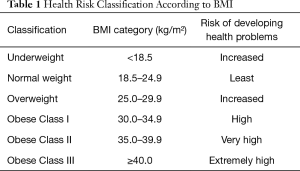
BMI and other measures for obesity grading and limitations
Lambert Adolphe Jacques Quetelet, a Belgian mathematician and statistician invented BMI, the most common and practical body weight classification formula, in the 1830s. BMI is a person’s weight in kilograms divided by the square of height in meters (39) (Table 1).
Full table
There are however, some subgroups that BMI is not appropriate such as; pregnant women, the elderly, young children, muscle builders and especially long distance athletes. The reason for this is because BMI doesn’t count the weight as muscle or fat.
Furthermore, the recent data also shows that BMI also doesn’t take into consideration the different types of fat, each of which can have different metabolic effects on health. It is accepted that visceral fat that develops deep among muscles and around organs, like the liver, is more harmful than subcutaneous fat (40,41). The adipose tissue is the primary site of excess energy and it also is an endocrine organ. Adipose tissue secretes certain hormones and other agents; it plays an important role on energy balance, immunity appetite regulation and much more. Some inflammatory mediators are secreted from the adipose tissue and these mediators play important roles on the development of cardio vascular disease (CVD), insulin resistance, T2DM and many more inflammatory diseases (41). Normal or even under- weighted people can have high levels of visceral fat. Although their BMI might be considered healthy, they may actually be at a higher risk of developing health problems.
The waist circumference is one of the other measures to classify the body weight, to gauge potentially harmful weight gain and fat depots. It is especially used for evaluating abdominal fat however, the evidence supporting this measurement and its ability to predict future health problems is still being investigated and is not lonely definitive enough (42).
CT scans and MRIs can give a better indication of visceral fat by separating out fat from muscle. Other types of scans, including dual-energy X-ray absorptiometry (DEXA) images, a method normally used to measure bone density, can also distinguish fat from bone and muscle mass. Although these are much more capable methods of prediction of the grade of obesity, the scans cost more than the prior methods (43).
Bariatric & metabolic: what is the correct nomenclature? Description designated
There still is an ongoing debate on the appropriate definition of the surgery for bariatric and metabolic procedures. Bariatric or obesity surgery was first defined in 1954 in an experimental animal model and with different types of resection models of small intestines. The investigators tried to evaluate the weight loss effects and the role of intestinal parts on weight maintenance or loss after operation (1). During that first description, different types of operations were defined and long-term results of those operations led us to know the effects of this surgery in more detail.
Weight loss was traditionally thought to be a result of the caloric restriction due to the reduced gastric volume from a restrictive based operation. In cases of malabsorptive ones, it is thought to be because of malabsorption of nutrients. However, recent studies showed that there might be a combination of several other factors that are effective on weight reduction after an operation. After a bariatric and metabolic surgery, it is expected that diabetes start to rapidly improve (in weeks or even days) before the process of significant weight loss. When comparing the similar weight loss results of diet versus bypass surgery, results regarding the anti-diabetic success revealed that a larger amount of improvement is with the surgery (44). Those findings and different animal models and hormonal studies suggest different pathways of weight-independent glucose-lowering effects of bariatric and metabolic surgery (45,46).
After the description of bariatric and metabolic surgery, which is still mostly used because of its simplicity, IFSO was suggested the use of “surgery for obesity and weight-related diseases” “Obesity and Metabolic Surgery” for the general name of these procedures. However, firstly, with different glucose-lowering mechanisms that are found everyday and secondly, with increasing consideration of surgery to treat diabetes in mildly obese individuals and even in merely overweight patients, the term ‘metabolic surgery’ is still and possibly will remain to be popular (47).
Operation selection for bariatric & metabolic surgery
The choice for bariatric surgery depends on different variables such as patient’s status of weight loss and/or metabolic control need, patient’s preferences, surgeon’s expertise, facilities and more. Still none of the different approaches for obesity and metabolic surgery has gained superiority over another. Laparoscopic sleeve gastrectomy (LSG), laparoscopic gastric bypass (RYGB), Laparoscopic adjustable gastric banding and laparoscopic biliopancreatic diversion/duodenal switch (BPD-DS) are the current, primary bariatric and metabolic procedures. LAGB and BPD-DS are the procedures that physicians should recommend by caution. LAGB has a high rate of unfavorable long-term weight loss and increased local complication rates. On the other hand BPD-DS is found to have greater associated nutritional risks related to the increased length of bypassed small intestine. Newer operations and concepts and tailored approaches still need more randomized trials and clinical evidence to get used in general surgical practice.
Current indications
What have changed over time? Obesity surgery guidelines throughout the years
Obesity became a main global health problem in the last decades.
It is certain that all clinical experiences and researches over the years show us that there are some clear circumstances for bariatric surgery indications and contraindications.
In 1978, National Institute of Health (NIH) Consensus Conference on Surgery for Obesity, considered intestinal (jejunoileal) bypass as the recommended obesity surgery procedure. However, this operation has proved to be effective in some reported series of cases, but it was associated with high number patients who experience serious complications. In 1978, the age limit for a surgery was 50 years old (48).
After this consensus, NIH published a newer statement on weight loss surgery in 1991. In that consensus meeting, Vertical Banded Gastroplasty (VBG) and Gastric Bypass operations are declared as the recommended operations for the treatment of obesity. Age limit was no longer quoted in the new consensus report.
In 2004, ASBS Consensus Conference for Bariatric Surgery for Morbid Obesity published a new statement on the advantages of laparoscopy for bariatric surgery (48), 2004 consensus also cleared out the obesity surgery for the adolescents and stated that a BMI that is greater than 40 kg/m2 (or 99.5th percentile for respective age) and at least one co-morbidity was a qualification for weight loss surgery in that age group (Table 2).

Full table
In 2008, according to the Interdisciplinary European Guideline on Surgery of Severe Obesity, bariatric surgery has proved to be the most effective treatment option for the morbid obese patients. In 2013, there was an update on the guideline, indicating that surgery can be performed to the following group of patients:
- 18 to 60 years old;
- With BMI more than 40 or;
- With BMI more than 35 with co-morbidities such as metabolic disorders, cardio-respiratory disease, severe joint disease, obesity-related severe psychological problems etc. (49).
Bariatric surgery is also recommended to patients who have failed an intense weight loss treatment program and started to gain weight.
T2DM is admitted as a reversible disease. As a result, bariatric surgery is accepted to be and effective method for remission of the T2DM. It was clarified that patients with BMI more than 30 and less than 35 may still be considered for bariatric surgery. The patients who lost weight and reached the weight less than required BMI with treatment program is not a contraindication for a planned surgery.
The contraindications for Bariatric Surgery:
- Absence of medical management;
- Non-stabilized psychotic disorders;
- Severe depression and/or personality disorders;
- Alcohol abuse and/or drug addiction;
- A life threatening disease in the short-term;
- Patients who are not able to care for themselves;
- Secondary diabetes and T2DM with positive antibodies (anti-GAD or ICA) or having less than 1 ng/mL c-peptide level or unresponsive to mixed meal challenge are contraindicated for bariatric surgery.
Metabolic surgeryOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
Increasing evidence show that GI surgical operations, including obesity operations, lead to nearly complete remission of T2DM. T2DM resolves only days after surgery with even no significant weight loss had occured. The types of surgeries performed for metabolic impairments mostly differ in wide spectrum. There is still lack of data and knowledge on the possible mechanisms of this T2DM remission that is independent from weight loss. Studies focused on alimentary tracts response after surgery, show promising data about gut hormones, microbiota and other various possible changes that might have an effect on this early remission. Besides the knowns in this topic, there are lots of unknown and undigested data, therefore, a consensus meeting was warranted.
In 2007, the first Diabetes Surgery Summit aimed to develop guidelines for the use of surgery to treat T2DM and conduct a base for future research. Many societies endorsed the meeting including, the American Diabetes Association (ADA), American Society for Metabolic and Bariatric Surgery (ASMBS), IFSO, European Association for the Study of Diabetes (EASD) and many other diabetes and surgery societies and associations (50).
The DSS-I defined the role of GI surgery in the treatment of T2DM in patients with severe obesity (BMI over 35 kg/m2). In carefully selected Class I obese patients (BMI: 30–35 kg/m2), surgical approach may also be appropriate as a non-primary alternative to treat inadequately controlled T2DM. With this report, it was emphasized that, for surgery in less obese or overweight, more research is expected with priority.
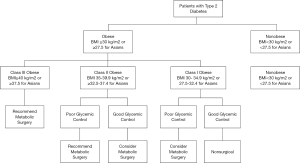
In September 2015, the second Diabetes Surgery Summit (DSS-II) was held in London, again endorsed by more than 40 medical and surgical societies. Between DSS-I and II, there was good evidence of RCTs and good quality prospective studies that showed positive short and long-term results of Class 1 obese patients following surgery. The DSS-II guidelines with its literature review and expert panels stated that “Metabolic surgery should be considered as an option to treat T2DM in patients with class 1 obesity, if patients are poorly controlled despite optimal medical treatment” (51).
Previously, medical care providers were not feeling confident to advise their patients on a surgical option for the treatment of T2DM. After the DSS-II recommendations, it was proven that metabolic surgery is an effective and in some circumstances, a more efficient tool for eligible patients. The algorithm for the patients with T2DM is now much more clear and promising (Figure 1).
Specific conditionsOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
Cancer
Surgical weight loss has shown to decrease the incidence of developing some types of cancers. Especially, breast, endometrial, prostate, colorectal and pancreas carcinomas are shown to be related with excess body fat and insulin resistance. With weight loss surgery and control of insulin resistance, the incidence of these cancer types decreases (52-55). On the other hand, the case when the patient has already diagnosed with cancer and referred for a possible bariatric and metabolic surgery remains controversial. Gagné DJ et al.reported 58 cancer patients in which 40 of them were diagnosed before the surgery, 2 patients during the surgery and 16 after the surgery. The study concluded that previous diagnosis of cancer is not a contraindication for obesity and metabolic surgery unless; the neoplastic disease is under control with no suspicion of recurrence and metastasis (56). Yet, the literature falls short for recommendations on this topic.
Chronic liver failure
Non Alcoholic Fatty Liver Disease (NAFLD) is a condition that clinically and histologically varies from simple fatty liver to cirrhosis. The stage when there is inflammation in NAFLD is called non-alcoholic steatohepatitis. These conditions occur in patients without history of alcohol abuse (57). NAFLD affects 25% of the global adult population in the world and increasing the mortality rate constantly (58).
The practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and the American College of Gastroenterology recommend that, in patients with obesity and NAFLD or NASH, bariatric surgery is not a contraindication unless established cirrhosis. The guideline concluded that it is still early to consider bariatric surgery as an option to treat NASH (59). In a large meta-analysis, it was shown that bariatric surgery improves steatosis and steatohepatitis in the majority of patients and improves or resolves liver fibrosis in 30% of patients (60).
Laursen et al. reported that, with bariatric surgery’s success on the improvement of GLP-1 and other gut hormones, important metabolic, inflammatory abnormalities, it might reverse the pathological liver changes in NAFLD and NASH patients. But there is need for large and randomized clinical trials with long-term follow-up to identify the precise role of bariatric surgery in NAFLD and NASH patients (61).
Psychiatric disorders
Mental health is a critical issue that should be interpreted before obesity and metabolic surgery. Preoperative psychiatry consultation should be warranted and a detailed psychiatric analysis should be performed. Due to anatomic and hormonal changes after the obesity and metabolic operations, patients should be mentally clear about the post-operative effects and the crucial changes that they have to make in their daily lives.
Some psychiatric conditions are known to be a contraindication for surgery whilst, in some other conditions the operations could be performed with adequate treatments. Severe and untreated bipolar disorder (62), schizophrenia and psychosis are the absolute contraindications of surgery. Moreover, due to the risk of increase in complications, patients with active substance or alcohol abuse and patients with Bulimia Nervosa should be evaluated and these disorders should also be interpreted as an absolute contraindication. However, after treatment and a reasonable period of remission of the symptoms, all of these patients could be re-examined with a psychiatry consultation and operation decisions could be re-evaluated (63). In all cases, the patient and the relatives should be informed about the symptom exacerbations that might occur during the post-surgical period. It is not yet clear that the exacerbations occurred in the normal course of the illness or impressed from surgery (64).
Another issue is the primary outcome of the Obesity and Metabolic Surgery, which is “surgical weight loss”. It was shown that, mood and anxiety disorders, binge eating disorder and night eating syndrome negatively affect the final weight loss outcome after the surgery. A multidisciplinary team should evaluate these disorders in the pre-operative and post-operative period, for reasonable and effective weight loss (49,53,65) (Table 3).

Full table
ConclusionsOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
Starting with the use of laparoscopy in bariatric surgery, the obstacle of Obesity and Metabolic Surgery was surpassed with less complications and better outcomes.
In the second step, especially in the last decade, controlled randomized studies were performed and various bariatric and metabolic societies supported the literature with numerous guidelines. The concept of metabolic surgery gains momentum and further strong argument. With the understanding of these operations’ effects, investigator and surgeons are now much more exited of what they are capable of.
However, with new findings and the changes in the world populations’ health concerns, we can estimate that more studies are needed to find the lesser complications with further outcomes.
AcknowledgmentsOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
Funding: None.
FootnoteOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mehmet Mahir Ozmen) for the series “Bariatric and Metabolic Surgery” published in Annals of Laparoscopic and Endoscopic Surgery. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ales-20-52). The series “Bariatric and Metabolic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Introduction
- Definitions of bariatric & metabolic surgery
- Metabolic surgery
- Specific conditions
- Conclusions
- Acknowledgments
- Footnote
- References
- Kremen AJ, Linner JH, Nelson CH. An experimental evaluation of the nutritional importance of proximal and distal small intestine. Ann Surg 1954;140:439-48. [Crossref] [PubMed]
- Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am 1967;47:1345-51. [Crossref] [PubMed]
- Griffen WO Jr, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg 1977;186:500-9. [Crossref] [PubMed]
- Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic Gastric Bypass, Roux-en-Y: Preliminary Report of Five Cases. Obes Surg 1994;4:353-7. [Crossref] [PubMed]
- Fobi MA, Fleming AW. Vertical banded gastroplasty vs gastric bypass in the treatment of obesity. J Natl Med Assoc 1986;78:1091-8. [PubMed]
- Mason EE. Vertical banded gastroplasty for obesity. Arch Surg 1982;117:701-6. [Crossref] [PubMed]
- Kuzmak LI. A Review of Seven Years' Experience with Silicone Gastric Banding. Obes Surg 1991;1:403-8. [Crossref] [PubMed]
- Madsbad S, Dirksen C, Holst JJ. Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol 2014;2:152-64. [Crossref] [PubMed]
- Rubino F, Nathan DM, Eckel RH, et al. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Diabetes Care 2016;39:861-77. [Crossref] [PubMed]
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract 2013;19:337-72. [Crossref] [PubMed]
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766-81. [Crossref] [PubMed]
- Vasileva LV, Marchev AS, Georgiev MI. Causes and solutions to "globesity": The new fa(s)t alarming global epidemic. Food Chem Toxicol 2018;121:173-93. [Crossref] [PubMed]
- Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery Worldwide 2013. Obes Surg 2015;25:1822-32. [Crossref] [PubMed]
- English WJ, DeMaria EJ, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 2018;14:259-63. [Crossref] [PubMed]
- Young MT, Gebhart A, Phelan MJ, et al. Use and Outcomes of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Gastric Bypass: Analysis of the American College of Surgeons NSQIP. J Am Coll Surg 2015;220:880-5. [Crossref] [PubMed]
- Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg 2010;252:319-24. [Crossref] [PubMed]
- Howard DD, Caban AM, Cendan JC, et al. Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg Obes Relat Dis 2011;7:709-13. [Crossref] [PubMed]
- de Jong JR, Besselink MG, van Ramshorst B, et al. Effects of adjustable gastric banding on gastroesophageal reflux and esophageal motility: a systematic review. Obes Rev 2010;11:297-305. [Crossref] [PubMed]
- Woodman G, Cywes R, Billy H, et al. Effect of adjustable gastric banding on changes in gastroesophageal reflux disease (GERD) and quality of life. Curr Med Res Opin 2012;28:581-9. [Crossref] [PubMed]
- Golomb I, Ben David M, Glass A, et al. Long-term Metabolic Effects of Laparoscopic Sleeve Gastrectomy. JAMA Surg 2015;150:1051-7. [Crossref] [PubMed]
- Hoyuela C. Five-year outcomes of laparoscopic sleeve gastrectomy as a primary procedure for morbid obesity: A prospective study. World J Gastrointest Surg 2017;9:109-17. [Crossref] [PubMed]
- Lager CJ, Esfandiari NH, Subauste AR, et al. Roux-En-Y Gastric Bypass Vs. Sleeve Gastrectomy: Balancing the Risks of Surgery with the Benefits of Weight Loss. Obes Surg 2017;27:154-61. [Crossref] [PubMed]
- Bloomberg RD, Fleishman A, Nalle JE, et al. Nutritional deficiencies following bariatric surgery: what have we learned? Obes Surg 2005;15:145-54. [Crossref] [PubMed]
- Goldner WS, Stoner JA, Lyden E, et al. Finding the optimal dose of vitamin D following Roux-en-Y gastric bypass: a prospective, randomized pilot clinical trial. Obes Surg 2009;19:173-9. [Crossref] [PubMed]
- Podnos YD, Jimenez JC, Wilson SE, et al. Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg 2003;138:957-61. [Crossref] [PubMed]
- Suter M, Calmes JM, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg 2006;16:829-35. [Crossref] [PubMed]
- Aarts EO, Dogan K, Koehestanie P, et al. Long-term results after laparoscopic adjustable gastric banding: a mean fourteen year follow-up study. Surg Obes Relat Dis 2014;10:633-40. [Crossref] [PubMed]
- Himpens J, Cadiere GB, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg 2011;146:802-7. [Crossref] [PubMed]
- Lemmens L. Banded Gastric Bypass: Better Long-Term Results? A Cohort Study with Minimum 5-Year Follow-Up. Obes Surg 2017;27:864-72. [Crossref] [PubMed]
- Baltasar A, Bou R, Bengochea M, et al. Duodenal switch: an effective therapy for morbid obesity--intermediate results. Obes Surg 2001;11:54-8. [Crossref] [PubMed]
- Marceau P, Biron S, Hould FS, et al. Duodenal switch: long-term results. Obes Surg 2007;17:1421-30. [Crossref] [PubMed]
- Biertho L, Simon-Hould F, Marceau S, et al. Current Outcomes of Laparoscopic Duodenal Switch. Ann Surg Innov Res 2016;10:1. [Crossref] [PubMed]
- Dorman RB, Rasmus NF, al-Haddad BJ, et al. Benefits and complications of the duodenal switch/biliopancreatic diversion compared to the Roux-en-Y gastric bypass. Surgery 2012;152:758-65. [Crossref] [PubMed]
- Bollig CA, Gilley D, Lesko D, et al. Economic Impact of Frozen Section for Thyroid Nodules with "Suspicious for Malignancy" Cytology. Otolaryngol Head Neck Surg 2018;158:257-64. [Crossref] [PubMed]
- Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg 2001;11:276-80. [Crossref] [PubMed]
- De Luca M, Tie T, Ooi G, et al. Mini Gastric Bypass-One Anastomosis Gastric Bypass (MGB-OAGB)-IFSO Position Statement. Obes Surg 2018;28:1188-206. [Crossref] [PubMed]
- Mahawar KK, Himpens J, Shikora SA, et al. The First Consensus Statement on One Anastomosis/Mini Gastric Bypass (OAGB/MGB) Using a Modified Delphi Approach. Obes Surg 2018;28:303-12. [Crossref] [PubMed]
- Shoar S, Poliakin L, Rubenstein R, et al. Single Anastomosis Duodeno-Ileal Switch (SADIS): A Systematic Review of Efficacy and Safety. Obes Surg 2018;28:104-13. [Crossref] [PubMed]
- Obesity: preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). World Health Organization, 2000.
- Ahima RS, Lazar MA. Physiology. The health risk of obesity--better metrics imperative. Science 2013;341:856-8. [Crossref] [PubMed]
- Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: an endocrine organ. Arch Med Sci 2013;9:191-200. [Crossref] [PubMed]
- Grievink L, Alberts JF, O'Niel J, G, et al. Waist circumference as a measurement of obesity in the Netherlands Antilles; associations with hypertension and diabetes mellitus. Eur J Clin Nutr 2004;58:1159-65. [Crossref] [PubMed]
- Kim YJ, Lee SH, Kim TY, et al. Body fat assessment method using CT images with separation mask algorithm. J Digit Imaging 2013;26:155-62. [Crossref] [PubMed]
- Cummings DE, Rubino F. Metabolic surgery for the treatment of type 2 diabetes in obese individuals. Diabetologia 2018;61:257-64. [Crossref] [PubMed]
- Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 2013;309:2240-9. [Crossref] [PubMed]
- Schauer PR, Bhatt DL, Kashyap SR. Bariatric surgery versus intensive medical therapy for diabetes. N Engl J Med 2014;371:682. [Crossref] [PubMed]
- Cummings DE, Cohen RV. Beyond BMI: the need for new guidelines governing the use of bariatric and metabolic surgery. Lancet Diabetes Endocrinol 2014;2:175-81. [Crossref] [PubMed]
- 2004 ASBS Consensus Conference on Surgery for Severe Obesity. Surg Obes Relat Dis 2005;1:297-381. [PubMed]
- Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg 2014;24:42-55. [Crossref] [PubMed]
- Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg 2010;251:399-405. [Crossref] [PubMed]
- Cohen RV, Shikora S, Petry T, et al. The Diabetes Surgery Summit II Guidelines: a Disease-Based Clinical Recommendation. Obes Surg 2016;26:1989-91. [Crossref] [PubMed]
- Pontiroli AE, Ceriani V, Sarro G, et al. Incidence of Diabetes Mellitus, Cardiovascular Diseases, and Cancer in Patients Undergoing Malabsorptive Surgery (Biliopancreatic Diversion and Biliointestinal Bypass) vs Medical Treatment. Obes Surg 2019;29:935-42. [Crossref] [PubMed]
- De Luca M, Angrisani L, Himpens J, et al. Indications for Surgery for Obesity and Weight-Related Diseases: Position Statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg 2016;26:1659-96. [Crossref] [PubMed]
- Winder AA, Kularatna M, MacCormick AD. Does Bariatric Surgery Affect the Incidence of Breast Cancer Development? A Systematic Review. Obes Surg 2017;27:3014-20. [Crossref] [PubMed]
- Winder AA, Kularatna M, MacCormick AD. Does Bariatric Surgery Affect the Incidence of Endometrial Cancer Development? A Systematic Review. Obes Surg 2018;28:1433-40. [Crossref] [PubMed]
- Gagné DJ, Papasavas PK, Maalouf M, et al. Obesity surgery and malignancy: our experience after 1500 cases. Surg Obes Relat Dis 2009;5:160-4. [Crossref] [PubMed]
- Younossi ZM, Marchesini G, Pinto-Cortez H, et al. Epidemiology of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: Implications for Liver Transplantation. Transplantation 2019;103:22-7. [Crossref] [PubMed]
- Younossi ZM. Non-alcoholic fatty liver disease - A global public health perspective. J Hepatol 2019;70:531-44. [Crossref] [PubMed]
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012;142:1592-609. [Crossref] [PubMed]
- Fakhry TK, Mhaskar R, Schwitalla T, et al. Bariatric surgery improves nonalcoholic fatty liver disease: a contemporary systematic review and meta-analysis. Surg Obes Relat Dis 2019;15:502-11. [Crossref] [PubMed]
- Laursen TL, Hagemann CA, Wei C, et al. Bariatric surgery in patients with non-alcoholic fatty liver disease - from pathophysiology to clinical effects. World J Hepatol 2019;11:138-49. [Crossref] [PubMed]
- Bauchowitz AU, Gonder-Frederick LA, Olbrisch ME, et al. Psychosocial evaluation of bariatric surgery candidates: a survey of present practices. Psychosom Med 2005;67:825-32. [Crossref] [PubMed]
- Friedman KE, Applegate K, Portenier D, et al. Bariatric surgery in patients with bipolar spectrum disorders: Selection factors, postoperative visit attendance, and weight outcomes. Surg Obes Relat Dis 2017;13:643-51. [Crossref] [PubMed]
- Shelby SR, Labott S, Stout RA. Bariatric surgery: a viable treatment option for patients with severe mental illness. Surg Obes Relat Dis 2015;11:1342-8. [Crossref] [PubMed]
- de Zwaan M, Enderle J, Wagner S, et al. Anxiety and depression in bariatric surgery patients: a prospective, follow-up study using structured clinical interviews. J Affect Disord 2011;133:61-8. [Crossref] [PubMed]
Cite this article as: Dilektasli E, Demir B. Definitions and current indications for obesity and metabolic surgery. Ann Laparosc Endosc Surg 2021;6:8.